and Chao-Hui Zheng1
(1)
Department of Gastric Surgery, Fujian Medical University Union Hospital, Fuzhou, China
3.1 Instruments
3.1.1 Routine Devices
A high-definition camera and display systems, a pneumoperitoneum machine, irrigation and suction devices, and video and image storage devices should be available, as well as routine laparoscopy equipment, such as 5–12-mm trocars, Maryland forceps, noninvasive grasping forceps, intestinal forceps, an aspirator, scissors, a needle holder, vascular clamps, an absorbable clip applier, a titanium clip applier, and small gauzes (Figs. 3.1, 3.2, and 3.3).




Fig. 3.1
Small gauzes

Fig. 3.2
An absorbable clip applier, a titanium clip applier, Maryland forceps, and a needle holder

Fig. 3.3
Gastric forceps, intestinal forceps, and an aspirator
3.1.2 Special Devices
Ultracision, LigaSure™ vessel sealing system, bi-active coagulation set, and all varieties of intestinal Endo-GIA and circular staplers should be at the ready.
3.2 Patient’s Position
Appropriate patient positioning is important for intraoperative exposure during laparoscopic gastrectomy for gastric cancer. The patient is usually placed in the supine position with legs separated. The surgical table is declined about 10–20° into the reverse Trendelenburg position. Therefore, the patient’s upper body is elevated. This causes the intestine to move toward the lower abdomen, thus helping to expose the upper abdomen (Fig. 3.4). When dissection of the splenic hilar lymph nodes (LNs) is performed, the patient’s upper body is elevated about 10–20°, and the left side of the body is tilted up about 20–30° (Fig. 3.5), allowing the intestine and omentum to move toward the right lower abdomen. This helps expose the splenic hilar area.



Fig. 3.4
The patient is in the supine and reverse Trendelenburg position

Fig. 3.5
The patient is in the reverse Trendelenburg and right lateral position
3.3 Surgeons’ Locations
Generally, the surgeon stands on the patient’s left side, the assistant is on the right side, and the camera operator is between the patient’s legs (Fig. 3.6), while during dissection of the splenic hilar LNs, the surgeon stands between the patient’s legs, with the assistant and camera operator both on the patient’s right (Fig. 3.7).



Fig. 3.6
Surgeons’ general locations

Fig. 3.7
Surgeons’ locations during the splenic hilar lymph node dissection
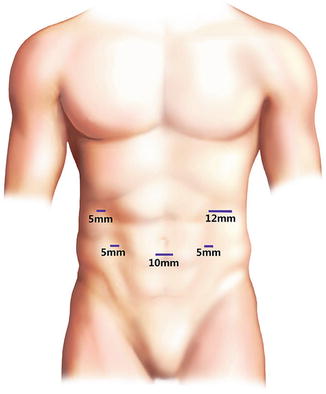
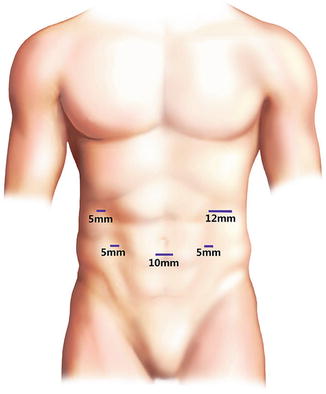
3.4 Location of Trocars
The 5-port method is generally used (Figs. 3.8 and 3.9). A 10-mm trocar is inserted 1 cm below the umbilicus as an observation port. Another 12-mm trocar is introduced in the left preaxillary line 2 cm below the costal margin as a major hand port. A 5-mm trocar is then inserted in the left midclavicular line 2 cm above the umbilicus as a tractive port. Two 5-mm trocars are severally placed in the right midclavicular line 2 cm above the umbilicus and in the right preaxillary line 2 cm below the costal margin as two accessory ports. The observation port is usually inserted first. For this insertion, an approximately 1.5-cm-long incision is made, and the abdominal wall is raised with towel forceps. When inserting the trocar, the operator should rotate it left and right and move it forward slowly. The sensation of the breakthrough “pop” indicates that the trocar has entered the abdominal cavity and the puncture sleeve is removed. Pneumoperitoneum should be established after trocar insertion is confirmed by laparoscopy to avoid subcutaneous emphysema. The remaining trocars should be inserted into the ports under the laparoscopic image.
 < div class='tao-gold-member'>
< div class='tao-gold-member'>




Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






