- Only a small proportion of patients attending general nephrology clinics will eventually progress to stage 5 chronic kidney disease (CKD).
- Up to 25% of patients starting renal replacement therapy do so without being previously known to renal teams. Such ‘crash landers’ have been shown to have poorer outcomes than those starting dialysis through dedicated pre-dialysis clinics. (See Chapter 13 and Appendix 4).
- Supporting patients through the huge changes associated with end-stage renal failure (ESRF) requires the input of a complex, dedicated multiprofessional team.
- Good education about their condition and their choices (including that provided by other patients) is key to empowering patients to take control of their health.
- Control of risk factors for progression of kidney disease and treatment of the extensive symptom burden associated with stage 5 CKD are important aspects of pre-dialysis clinical management.
- Patients should be given the full range of dialysis choices and supported in making an individual choice most suitable to their health and lifestyle.
- Some older, frailer patients may feel that the burden of dialysis is too great—they should continue to receive specialized care in the maximal supportive care pathway focusing on symptom relief and planning of where and how they would like to be looked after at the end of their life.
- For those in whom it is possible, priority should be given to work up for a pre-emptive living donor transplant but all suitable patients should undergo work up for activation on the cadaveric transplant list.
- The decision for a patient to start dialysis usually reflects a combination of increasing uraemic symptoms and increasingly abnormal biochemistry.
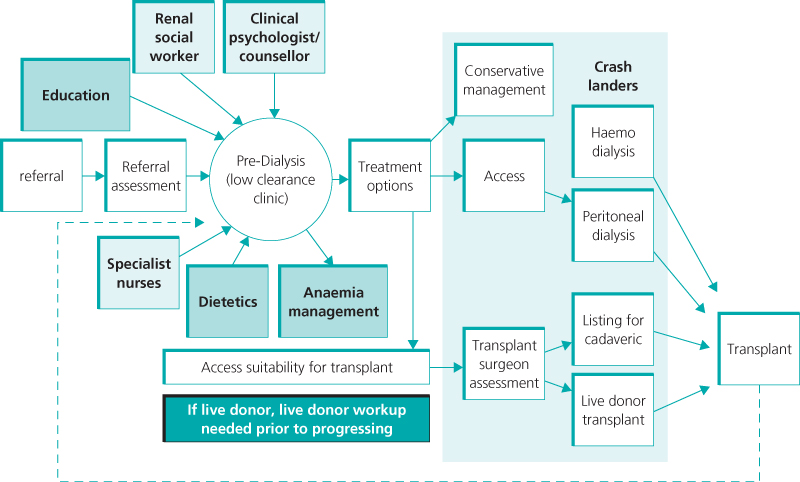
Every year, a small proportion of patients attending general nephrology clinics will progress to the point where clinicians feel that end-stage renal failure (ESRF) is likely within the next year. Dedicated pre-dialysis (or low clearance) clinics (LCCs) have been introduced in the last 15 years to deliver well-organized, patient-focused, multidisciplinary team care to improve their dialysis, transplantation and conservative care outcomes. The team consists of nephrologists, surgeons, nurses, dieticians, counsellors and social workers, who provide holistic care by focusing on correction of chronic kidney disease (CKD) complications, cardiovascular risk management, patient education and early preparation for renal replacement therapy (RRT) or maximal conservative care (Figure 4.1).
Figure 4.1 Pathway from nephrology to RRT.
(Source: Adapted from NHS Institute for Innovation and Improvement publication
For some patients (such as those with a family history of adult polycystic kidney disease who have seen family members reach ESRF), this phase of care is an inevitable and expected progression of their renal journey. For many others, who have previously understood their kidney disease to be relatively minor, this is the first point at which they realize the very significant effect their kidney disease will have on their lifestyle, their employment and their family.
Various studies have demonstrated that early referral to pre-dialysis clinics is associated with:
Additional benefits include:
The (2004) National Service Framework for Renal Services’ guidelines recommend that patients whose estimated glomerular filtration rate (eGFR) is < 30 mL/min/1.73 m2 (CKD stages 4–5) and declining be referred to the pre-dialysis (low clearance) clinic at least a year before RRT is needed. In clinical practice, most nephrologists refer patients to pre-dialysis clinics with a creatinine clearance of < 15–20 mL/min and falling or an expected start of RRT within 6–12 months.
In this chapter, the different roles of the pre-dialysis team in providing optimal, high-quality care to patients approaching ESRF will be discussed (Figure 4.1).
Education
Extensive patient education is central to optimal pre-dialysis care and uses various measures (comprehensive and culturally appropriate information booklets, DVDs/CDs, education days and one-to-one visits, Figure 4.2). Patients, families and carers attend multidisciplinary group education days. Education may begin with a basic explanation of where the kidneys are located in the body and what functions they perform, right up to explaining the various medications and treatment options, including dialysis, transplantation and maximal conservative care (see Chapters 9, 10 and 11). Patients are taught how to understand their own blood test results and are given talks on diet and anaemia management in renal failure. Such sessions also give patients the opportunity to meet other patients who may be approaching dialysis or who are already receiving renal replacement therapy, thus facilitating adjustment and normalization of their diagnosis. There is evidence that patients participating in education programmes have improved psychological and social outcomes. All the above measures help to facilitate informed involvement in the decision-making progress and encourage self-management and home dialysis therapies (see Chapter 10), thus allowing patients to take a degree of control over living with a chronic condition. Unfortunately, a small proportion of patients struggle to accept their prognosis and thus refuse or are unable to participate in education sessions or the decision-making process. Varied strategies should be employed to engage patients who are in denial, such as the use of peer supporters and motivational interviewing techniques, but expert communication skills used with persistence, sensitivity and empathy provide the best basis from which to develop trusting constructive relationships with all patients.
Post-dialysis education is also important to ‘crash landers’ who enter the system as emergencies within 90 days of requiring RRT (and often in immediate need of RRT) and subsequently have poorer outcomes. The pre-dialysis team provide education to this group to lessen the adverse effects and ensure that they are also given the choice to move onto self-care therapies rather than automatically remaining on their initial therapy, which is usually HD.
Preservation of Existing Renal Function and Reduction of Cardiovascular Risk Factors
The rate of decline of renal function varies between patients and depends on the cause of the primary disease, race and the presence of exacerbating factors. Cardiovascular morbidity and mortality are significant in patients with stages 4 and 5 CKD.
In the pre-dialysis clinic, many factors are addressed to preserve existing renal function and to reduce cardiovascular risk (Table 4.1).
Table 4.1 Factors for preserving renal function and reducing cardiovascular risk
ACE, angiotensin converting enzyme; NSAIDs, nonsteroidal anti-inflammatory drugs.
| Risk factor for progression of CKD or cardiovascular risk | Intervention | Target value (where applicable) |
| Hypertension | Control with salt and fluid restriction, exercise, antihypertensive medications | < 140/90 mmHg in patients with CKD |
< 130/80 mmHg in patients with CKD and diabetes or proteinuria  1 g 1 g | ||
| Hyperglycaemia | Dietary advice, weight reduction, oral hypoglycaemics and insulin | HbA1c < 7.5% without frequent hypoglycaemic attacks |
| Dyslipidaemia | Dietary advice, statins | Total cholesterol < 4 mmol/L for secondary prevention and diabetes |
| Total cholesterol < 5 mmol/L for others | ||
| Acidosis | Supplementation with oral bicarbonate | Maintain serum bicarbonate levels over or at 22 mmol/L |
| Minimize proteinuria | ACE inhibition, angiotensin receptor inhibition | Urinary protein levels of < 0.5 g/24 h |
| Nephrotoxic drugs | Avoid NSAIDs, trimethoprim and radiological or angiographic contrast media. |
All patients should also be encouraged to adopt a healthy lifestyle with cessation of smoking, increased exercise and a target BMI of 20–25. Careful liaison with colleagues in urology, cardiology, vascular surgery and radiology is needed to ensure avoidance/minimization of radiological contrast and prompt treatment of urinary obstruction. Additional measures to reduce adverse cardiovascular outcomes include antiplatelet therapy (if estimated 10-year risk of cardiovascular disease > 20%), treating anaemia (which can lead to left ventricular hypertrophy) and treating mineral bone disorders.
Addressing Complications of Chronic Kidney Disease
Management of Fluid Overload
Salt and fluid overload is common and leads to hypertension, peripheral and pulmonary oedema (Figure 4.3). Measures to control fluid overload include salt and fluid intake restriction (1–1.5 L/day) and the use of diuretics (furosemide, metolazone) while monitoring the patient’s weight, blood pressure (BP), electrolyte and renal function to avoid over-diuresis.
< div class='tao-gold-member'>