| 9 | Polyps and Polyposis Syndromes |
Polyps
 Definition
Definition
The term “polyp” describes a mass of tissue protruding into the lumen of the bowel, without implying pathological relevance. Polyps can be stalked, round, or sessile and can vary in size. They can occur as solitary or multiple polyps. Polypoid lesions are the most common pathological finding of colonoscopy. Polyps can only be classified by histological evaluation.
Pathologically and anatomically, polyps of epithelial tissue are distinguished from those of mesodermal tissue and there are also a few other special forms. Table 9.1 shows the WHO classification of colorectal polyps. According to WHO guidelines, epithelial polyps are divided into neoplastic and nonneoplastic (tumorlike) polyps, whereby neoplastic polyps make up some 70% of all colorectal polyps (3).
Neoplastic polyps | Nonneoplastic (tumorlike) polyps |
|---|---|
|
|
Bowel segment | Percentage of colorectal polyps |
|---|---|
Cecum | 4% |
Ascending colon | 10% |
Hepatic flexure | 3% |
Transverse colon | 9% |
Splenic flexure | 2% |
Descending colon | 8% |
Sigmoid colon | 30% |
Rectum | 34% |
Histology | Percentage of all polyps | Malignant transformation at diagnosis up to |
|---|---|---|
Tubular | 75% | 4.8% |
Tubulovillous | 15% | 19.0% |
Villous | 10% | 38.4% |
 Clinical Picture and Clinical Significance
Clinical Picture and Clinical Significance
Epidemiology. The prevalence of colorectal polyps varies greatly in different regions of the world, though it tends to be higher in western industrialized nations with high standards of living. Colon polyps are, on the whole, very common and their frequency increases with age. Some 70% of all colon polyps are adenomas, and 65 % of these are located between the rectum and splenic flexure. Between 30-50 % of patients with adenomas have several adenomas simultaneously; the most significant factor determining the presence of an adenoma is being older than 60 years of age. Table 9.2 shows the approximate distribution of colorectal polyps by intestinal segment (3).
Symptoms. Most polyps do not cause any symptoms. Possible symptoms include anal bleeding (unexplained iron deficiency anemia) and signs of obstruction accompanied by abdominal pain (larger polyps). Villous adenomas have a special status related to their clinical picture as they can secrete a watery potassium-rich secretion, occasionally up to several liters per day. The patient thus suffers from watery diarrhea and mucous discharge; laboratory tests may detect hypokalemia.
Adenoma–dysplasia–carcinoma sequence. Adenomas deserve special attention as they make up 70 % of all colon polyps. An adenoma is a benign neoplastic epithelial tumor in which cells arise from glandular epithelium with varying degrees of dysplasia and varying potential for malignant transformation. Current opinion holds that every adenoma has the potential to become a carcinoma (adenoma–dysplasia–carcinoma sequence). The “National Polyp Study” and the Erlangen Registry of Colorectal Polyps have identified adenoma size and polyp histology as independent risk factors in the development of a carcinoma (3, 5). The rate of malignancy increases with increasing size: at 2 cm and larger, 12% of adenomas have high-grade dysplasia and 33% of adenomas contain carcinomatous components. The relationship between histology and transformation of various epithelial polyps is shown in Tab. 9.3.
Atypical cells can be found in 10% of all adenomas, whereby initial proliferation is limited to a small area of the polyp. Later, the malignant cells spread, infiltrating the polyp stalk, and, finally, the intestinal wall.
 Diagnosis
Diagnosis
Family history and clinical findings form the basis for diagnosis. Family history is especially important for hereditary forms of polyposis syndrome and where there is a family history of colorectal adenomas and carcinomas. Digital rectal palpation makes an important contribution to clinical findings, but it only detects only around 5-10% of polyps. Occult blood tests are not suitable as a primary screening tool for adenomas, as their sensitivity for adenomas is only 30%. Occult blood tests are negative for 93% of colon adenomas up to 1 cm in size and for 77% of adenomas 1-2 cm in size, whereby 7% of polyps of this size are malignant. Twenty-five percent of polyps larger than 2 cm escape detection and of these up to 45% are already transforming malignantly.
Role of endoscopy. Endoscopy, i.e., total colonoscopy, is essential and it is the main diagnostic tool. Endoscopy is the most informative method of diagnosing colorectal polyps. Endoscopic biopsy—or ectomy—of polyps initially has a purely diagnostic role. Not until the results of histological evaluation are available can it be decided whether endoscopy is the definitive treatment method or whether other treatments (removal of remaining polyp pieces, surgical intervention) are required. Early-stage polyps can be detected and removed endoscopically, thereby reducing the incidence of carcinoma.
Complementary procedures. Barium enemas can be used complementarily, e.g., for strictures, endoscopically impassable segments, or in cases where endoscopy is not possible. Contrast enemas should only be administered using double-contrast technique; false negative findings occur in 2-22% of patients using this technique, depending on size.
The role of virtual colonoscopy in diagnosing colon polyps remains unclear. Virtual colonoscopy can, however, hardly replace conventional colonoscopy as a screening tool: sensitivity for adenomas <5mm is around 30-50%; for adenomas 6-9 mm, sensitivity is at the most 80% and for adenomas > 1 cm ca. 90% (2). In more recent studies, results of virtual colonoscopy are even less impressive: the rate of detection of polyps > 1 cm is reported at 70% and among polyps 5-9 mm at only 40-60% (4). Thus, for polyps detected by virtual colonoscopy, conventional colonoscopy is absolutely essential for ectomy of the polyp; currently 20% of detections are false positives (2).
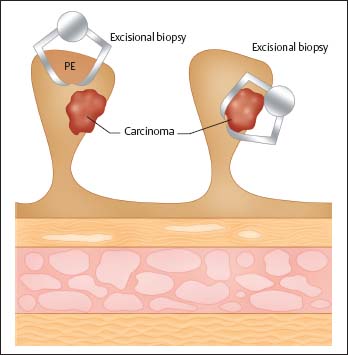
Fig. 9.1 Problem of forceps biopsy for polyps with and without car-cinomatous components.
Follow-up studies on colon polyps (using double-contrast techniques) are available from “precolonoscopy” times. Of polyps larger than 1 cm, 37% grew in size during an observation period of nine years; cumulative carcinoma risk after five, 10, and 20 years was 4%, 14%, and 35 % respectively (10). Based on these data, total polypectomy is indicated for all colon polyps larger than 5 mm (10), since differentiation between adenomas and adenocarcinomas is not possible based on biopsy alone (Fig. 9.1). Histological evaluation is essential for every resected polyp and must include histological classification, degree of in- traepithelial neoplasia and report of excisional biopsy. Chapter 18 goes into more detail concerning polypectomy technique.
 9.1 Diminutive polyps
9.1 Diminutive polyps
a-c Small adenomas, less than 5 mm, covered by apparently normal mucosa, flat, sessile.

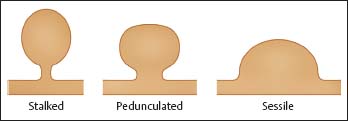
Fig. 9.2 Macroscopic growth forms of colorectal adenomas.
Prospective colonoscopy studies have shown that if polyps smaller than 5 mm without adenoma components (hyperplastic polyps) are detected in the rectum or sigmoid colon, the prevalence of metachronous adenomas in proximal colon segments is 24-34% (1). Thus, distal hyperplastic polyps can be considered index lesions for more proximal metachronous adenomas.
Epithelial Polyps
Adenomas. Typical appearance of colon adenomas varies. Differentiating between an adenoma and a hyperplastic polyp is only possible using special endoscopic techniques, in particular, chromoendoscopy and “pit pattern classification” (see Chapter3).



















 The smallest adenoma can measure less than 5 mm, is covered by normal-appearing mucosa, and is flat and sessile, located on the mucosal surface, and occasionally appearing reddish in color. Polyps < 5 mm are referred to as “diminutive polyps” (
The smallest adenoma can measure less than 5 mm, is covered by normal-appearing mucosa, and is flat and sessile, located on the mucosal surface, and occasionally appearing reddish in color. Polyps < 5 mm are referred to as “diminutive polyps” ( 9.1). Histologically, they are characterized by closely situated, branchlike tubuli, surrounded by lamina propria. Larger adenomas are characterized as sessile or stalked: sessile adenomas have a broad base, while stalked adenomas have a type of stalk of varying length (
9.1). Histologically, they are characterized by closely situated, branchlike tubuli, surrounded by lamina propria. Larger adenomas are characterized as sessile or stalked: sessile adenomas have a broad base, while stalked adenomas have a type of stalk of varying length (






