| 18 | Polypectomy and Mucosectomy |
 Indications and Contraindications
Indications and Contraindications
Endoscopic polypectomy of colorectal polyps is indicated by clinical symptoms (to the extent that they are present) such as bleeding or occlusion and/or early detection or prevention of cancer. Table 18.1 lists indications and contraindications for endoscopic polypectomy. If the patient has any contraindications, the potential risks of polypectomy must be weighed against expected diagnostic or therapeutic benefit (3). In such cases, procedures must be performed on an in-patient basis or with appropriate postoperative surveillance. Colonoscopic polypectomy involves significantly lower morbidity, mortality, and costs than comparable surgical resection. If an experienced endoscopist is unable to remove safely or completely a polyp, then laparotomy or laparoscopic polypectomy are indicated (3). The aim of polypectomy can be viewed as primarily diagnostic: complete removal of colorectal polyps for definitive histological diagnosis, evaluation of their nature, and thus assessment of further therapeutic measures.
 Preparing for Polypectomy and Mucosectomy
Preparing for Polypectomy and Mucosectomy
Patient preparation for colonoscopy and polypectomy, including bowel cleansing, is performed according to standardized procedures (see also Chapter 1 “Preparing for the Examination”. The patient should be prepared for an i. v. line before intervention.
Clotting status, platelet aggregation inhibitors, and anticoagulants. In addition to relevant patient medical information for colonoscopy (see also Chapter 1), knowledge of the patient’s current clotting status is also essential. According to DGVS (German Society of Digestive and Metabolic Diseases) guidelines, prothrombin time/INR should be above 50%; platelet count should be above 50000/mm3; and partial thromboplastin time should not be longer than double the norm (3). It should be noted that patients with thrombocytopenia are at risk of bleeding even at levels considerably higher than 50000 thrombocytes/mm3.
Patients taking platelet aggregation inhibitors and patients receiving dialysis treatment have an increased bleeding tendency even when clotting parameters are normal. This is not a contraindication. For routine polypectomies, patients should discontinue use of platelet aggregation inhibitors including substances containing acetylsalicylic acid or clopidogrel one week prior to the procedure (8). In individual patients, however, where the risk of discontinuing use is greater or where medication is absolutely necessary due to underlying disease, continued use may be considered after discussion with the patient.
Patients taking Marcumar for a limited period of time should postpone elective intervention until after discontinuation of anticoagulation therapy. If long-term Marcumar use is necessary, the patient must be switched to unfractionated heparin in an in-patient procedure. Heparin should not be administered less than six hours (at the latest, four hours) before the procedure begins. Use can be resumed two to six hours after examination. Low molecular weight heparin should not be used at all on the day of examination.
Indications | Contraindications |
|---|---|
|
|
Antibiotic prophylaxis. Indications for prophylactic antibiotics are determined based on overall risk of endocarditis and bacteremia resulting from polypectomy. It should be noted that polypectomy is associated with only a low risk of bacteremia. Patients with a high risk of endocarditis should receive an antibiotic prophylaxis prior to polypectomy. Prophylactic antibiotics are not mandatory for patients with a moderate risk of endocarditis.
 Instrumentation
Instrumentation
Endoscopic polypectomy techniques using a high frequency current (high frequency diathermy) with a larger patient plate placed on the thigh (neutral electrode) and a second (active electrode), smaller one (polypectomy snare), are highly standardized (3, 8). Electrical isolation of the patient must be ensured; the patient may not come into contact with any metal parts of the examining table during polypectomy. Patients with pacemakers require ECG monitoring and a defibrillator must be immediately available and ready for use. A pacemaker check should be performed as soon as possible following endoscopic therapy (i. e., same day). An overview of necessary accessories and technical requirements for polypectomy and mucosectomy of colon polyps is provided in the following box (8).
 Polypectomy
Polypectomy
Polyps are routinely removed during colonoscopy. Thus, around 95% of all polyps are removable without invasive surgical procedures. Polyps smaller than 5mm are removed with forceps; all others are removed with a snare (3). Despite safe and effective techniques for removing almost all colon polyps, deciding whether a particular polyp should be endoscopically resected and actually performing the procedure require a great deal of experience.
Complications are to be expected for endoscopic polypectomy of polyps with a base measuring >3 cm in diameter. Polyp size, however, is only a relative contraindication for endoscopic resection; larger polyps can be removed with so-called “piecemeal” techniques in some cases. Prior to endoscopic polypectomy, the polyp must be closely inspected in its entirety with base and stalk. This may require manipulation with a biopsy forceps, especially in the case of a malignant polyp in order to test whether it can be depressed against the bowel wall and thus check the potential for endoscopic polypectomy. If the polyp is localized in one of the flexures, or another area where visualization is difficult, it may be helpful to change the patient’s position.
If there are several polyps, they can usually be removed in one session. Large numbers of polyps may have to be resected one area at a time over several sessions; for several larger polyps, numerous sessions may help to avoid massive complications such as simultaneous perforations at various resection sites.
In general, proximally located polyps are resected and retrieved first. The colonoscope is then withdrawn to the more distal polyp, which is then removed. If the retrieval of a large, proximal polyp requires complete withdrawal of the colonoscope, the instrument must again be advanced to the height of the resected polyp and then slowly withdrawn to the deeper polyp and positioned.
Histological evaluation of all polyp fragments is necessary for precise diagnosis. If retrieval of all polyp pieces is not complete at the end of the examination, remaining polyp pieces can be retrieved from evacuated fluid with a sieve (Fig. 18.1).
 18.1 Instrumentation for endoscopic polypectomy and mucosectomy
18.1 Instrumentation for endoscopic polypectomy and mucosectomy

a Various types of polypectomy snares (left to right): symmetrical, hexagonal, oval, extra large snare. These snares have a diameter of 2.5 cm and are selected according to the type of polyp being resected. The extra large snare is for giant polyps; maximum snare diameter is 6 cm.

b Mucosectomy snares (left to right): for stenosis (cap technique, 2.5 cm diameter), monofilament snare for flat polyps (2.5 cm diameter), reinforced snare (5 cm diameter).

c Special suction caps for “suck-and-cut” method. The diameter of the suction caps is 17.2 mm.

d Instruments (left to right) for polyp retrieval: normal polypectomy snare, grasping forceps, four-pronged grasping forceps, dormia basket.

e Polyp trap device. The specimen bag is placed in the trap so that suctioned polyp fragments or small polyps remain hanging in the bag. The bag is cut open with scissors to retrieve the polyp fragments.

f Polyp retrieval net. The net is placed over the working channel of the instrument and the polyp or polyp pieces are caught in the net. The polyps are retrieved on withdrawing the instrument.
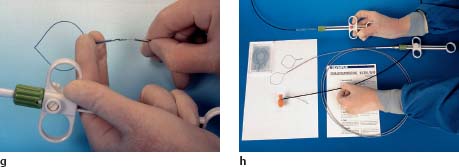
g, h Endoloop (detachable nylon snare). The detachable snare is tightened after being placed on the polyp stalk, closed, and later falls off.

i Hemoclips for mechanical hemostasis.

Fig. 18.1 Polyp sieve. By allowing stool to pass through a sieve, polyps or polyp pieces lost during endoscopic retrieval can be retrieved after examination.
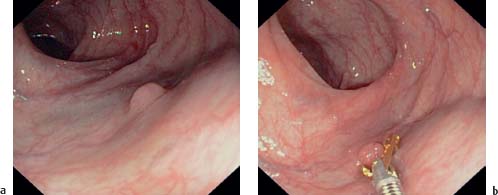
Fig. 18.2a, b Resection of a diminutive polyp (<5 mm) with grasping forceps.
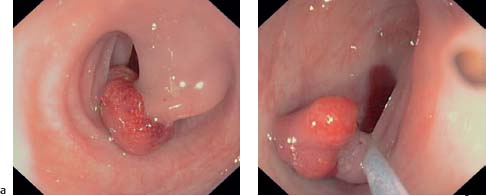
Fig. 18.3a, b Polyp with prominent stalk. Positioning the polypectomy snare around the polyp stalk. The level of transection or coagulation of the stalk is closer to the polyp head than to the bowel wall.

Fig. 18.4 Polyp stalk treated with hemoclips after rebleeding.
Small Polyps
According to guidelines of the German Society of Digestive and Metabolic Diseases (DGVS) (3) polyps <5mm are removed using biopsy forceps; attempted snare polypectomy usually “burns” the polyp, rendering histological evaluation impossible (Fig. 18.2). The small polyp should be repeatedly grasped with the forceps until it appears macroscopically to have been completely removed. This method entails the risk, however, that macroscopically undetectable polyp pieces may remain and could cause residual polyps. For this reason, some authors prefer the hot-biopsy forceps method (8), which enables the retrieval of histologically valuable material while coagulating the base of the resection site. However, this method entails risk of rebleeding and perforation.
Stalked Polyps
It should be possible to remove stalked polyps of any size in a single session using a snare.
Ensnaring the polyp head and positioning the snare. An appropriate snare is selected, looped around the polyp head, and then positioned around the stalk. The level of transection or coagulation should be closer to the polyp head than to the bowel wall (Fig. 18.3). Transection too close to the bowel wall may cause perforation; also, if rebleeding occurs from the remaining stalk, endoscopic hemostasis using injection or application of hemoclips is much easier with more remaining stalk (Fig. 18.4). The snare should not be closed until it is exactly at the transection line. Closing the snare too firmly before diathermy can “guillotine” the polyp stalk and cause bleeding. Polypectomy must always be performed under visualization: insufficient visualization can result in perforation of the bowel wall. If the polyp head is so large that even a giant snare cannot be looped around it, it should be removed in several pieces or portions (“piecemeal” polypectomy). This can reduce the size of the polyp head so that the snare can then be placed around the stalk and the polyp can be safely and completely removed.
Coagulation of the polyp stalk.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree















 18.1a, b),
18.1a, b),
 18.1c),
18.1c),
 18.1d), trap device (
18.1d), trap device (  18.1e), polyp net (
18.1e), polyp net ( 18.1f),
18.1f),
 18.1g, h),
18.1g, h),
 18.1i),
18.1i),











