Fig. 5.1
Small renal pelvic tumour, not detected by CT scan
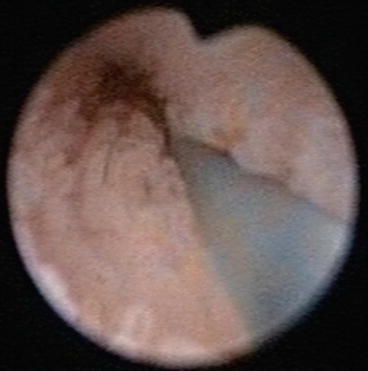
Fig. 5.2
Low papillary growth in the ureter, not detected by CT scan

Fig. 5.3
Prominent papilla
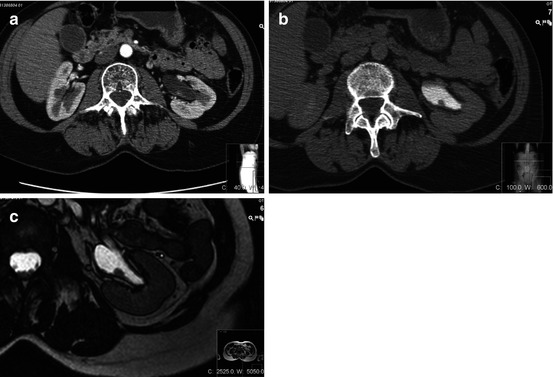
Fig. 5.4
(a) Renal pelvic tumour visualised in CT artery phase; (b) in the CT scan excretion phase, the tumour appears superficial; (c) by MRI it seems even more obvious that the tumour is superficial. However, the patient was operated on by radical nephroureterectomy, and pathology revealed that the tumour was high grade. Six months after the surgery, the patient was dead
5.7 Indications for Ureterorenoscopy
By ureterorenoscopic examination, using semirigid and flexible ureteroscopes, ureter, renal pelvis and calyces can be explored and biopsies and selective cytology can be obtained. Indications for diagnostic ureterorenoscopy are:
Suspicious radiographic findings in the UUT with or without malignant cells in bladder cytology.
Malignant cells in bladder cytology without diagnosed malignancy in the bladder.
Macroscopic haematuria from the UUT without radiographic findings.
In the latter case, one single episode of macroscopic haematuria with no malignant cells found in urine cytology and no radiographic findings in a low-risk patient does not require diagnostic ureteroscopy. However, if persistant bleeding or in a high-risk patient (heavy smoker, previous bladder cancer, occupational risk), diagnostic ureteropyeloscopy should be performed. The patient should be prepared for simultaneous laser treatment if tumours, suitable for localised treatment, are found.
If possible, a diagnostic and therapeutic ureterorenoscopy should be performed through a retrograde approach. The reason for this is that a percutaneous puncture may imply seeding of tumour cells in the access tract. However, in some cases, an antegrade or combined approach is needed. Such situations may be when a tumour is located in a lower calyx that cannot be reached via ureteroscopic retrograde approach or when a patient has been operated on with urinary diversion. Reimplanted ureters and ureteric strictures caused by other reasons such as radiation therapy may make it impossible to use a retrograde approach. The technical aspects will be further discussed in Chap. 18.
5.8 Treatment and Indications
The standard therapy for TCC in the UUT is radical nephroureterectomy. The reason is that the recurrence rate is relatively high, the sensitivity of cytology, as previously mentioned, is not very reliable and the radiographic methods not very sensitive for small tumour lesions. However, in patients with a solitary kidney or with severe renal failure, this will inevitably lead to haemodialysis, a condition with severe impact on the quality of life and on the costs for the society.
Consequently, indications for organ-sparing endoscopic treatment of TCC in the UUT are solitary kidney and kidneys with severely impaired function. A total renal function with a clearance <10 ml/min is not sufficient to avoid haemodialysis. Therefore, these patients should be offered an organ-sparing treatment. The option of radical nephroureterectomy should also be offered to the patient; however, the patient has to be informed that he or she cannot come into consideration for a renal transplant until after 5 years of no tumour recurrence. Moreover, in some countries, patients over the age of 70 are not eligible for renal transplantation. Another absolute indication is the presence of severe comorbidities, considered a contraindication for radical nephroureterectomy. Endoscopic organ-sparing treatment is less burdening for the patient and can usually be carried out in spinal anaesthesia in those cases.
References
1.
2.
3.
4.
El-Nahas AR, Shoma AM, Eraky I et al (2006) Percutaneous endopyelotomy for secondary ureteropelvic junction obstruction: prognostic factors affecting late recurrence. Scand J Urol Nephrol 40:385–390PubMedCrossRef
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








