According to the World Health Organization, there are approximately 2 billion annual cases of diarrhea worldwide. Diarrhea is the leading cause of death in children younger than 5 years and kills 1.5 million children each year. It is especially prevalent in the developing world, where mortality is related to dehydration, electrolyte disturbance, and the resultant acidosis, and in 2001, it accounted for 1.78 million deaths (3.7% of total deaths) in low- and middle-income countries. However, diarrhea is also a common problem in the developed world, with 211 million to 375 million episodes of infectious diarrheal illnesses in the United States annually, resulting in 73 million physician consultations, 1.8 million hospitalizations, and 3100 deaths. Furthermore, 4% to 5% of the Western population suffers from chronic diarrhea. Given the high prevalence of diarrhea, research has been directed at learning more about the cellular mechanisms underlying diarrheal illnesses in order to develop new medications directed at novel cellular targets. These cellular mechanisms and targets are discussed in this article.
According to the World Health Organization, there are approximately 2 billion annual cases of diarrhea worldwide. Diarrhea is the leading cause of death in children younger than 5 years and kills 1.5 million children each year. It is especially prevalent in the developing world, where mortality is related to dehydration, electrolyte disturbance, and the resultant acidosis, and in 2001 it accounted for 1.78 million deaths (3.7% of total deaths) in low- and middle-income countries. However, diarrhea is also a common problem in the developed world, with 211 million to 375 million episodes of infectious diarrheal illnesses in the United States annually, resulting in 73 million physician consultations, 1.8 million hospitalizations, and 3100 deaths. Furthermore, 4% to 5% of the Western population suffers from chronic diarrhea. Given the high prevalence of diarrhea, research has been directed at learning more about the cellular mechanisms underlying diarrheal illnesses in order to develop new medications directed at novel cellular targets. These cellular mechanisms and targets are discussed in this article.
Mechanisms of diarrhea
Ingestion of fluids and secretion of salivary, gastrointestinal, and pancreatic juices result in up to 10 L of fluid passing through the small intestinal lumen daily. A maximum of 16 L/d and 5 L/d can be absorbed in to the small intestine and colon, respectively. Normally, secretion and absorption of fluids are tightly regulated. Diarrhea develops when the balance between secretion and absorption is disrupted, and in adults, diarrhea has been defined as a stool output of 200 mL or more per day. Patients typically complain of increased stool frequency, reduced stool consistency, and urgency. Diarrhea can be defined as secretory, osmotic, or due to disordered motility. Secretory diarrhea results from excessive secretion or reduced absorption of water and electrolytes by epithelial cells, usually with little structural damage. Secretory diarrhea is commonly caused by some microbial infections, gastrointestinal hormone–producing tumors, and inflammatory mediators (eg, prostaglandins). Osmotic diarrhea occurs when there is an excessive luminal osmotic load, causing retention of water in the intestinal lumen. Osmotic diarrhea typically occurs in 2 situations: ingestion of a poorly absorbed substrate (eg, laxative use, mannitol, sorbitol) or malabsorption (eg, lactase deficiency, celiac disease). Disordered motility can lead to accelerated transit, reducing the ability of the gastrointestinal tract to absorb water and nutrients. Hyperthyroidism and irritable bowel syndrome can cause diarrhea via this mechanism.
Ion Secretion
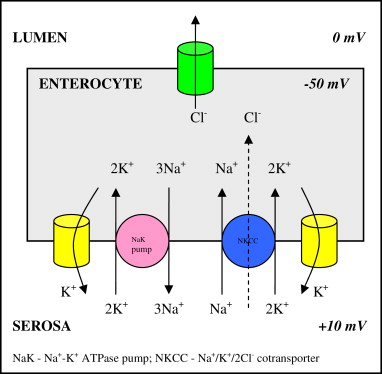
Epithelial cells form an impermeable and selective barrier, adjoined to each other by tight junctions that act as selective pores, thus determining the permeability of the membrane. Intestinal fluid secretion results predominantly from the active secretion of chloride and bicarbonate ions. Chloride secretion relies on 4 membrane transport complexes: the apical chloride channel, the basolateral potassium channel, the sodium-potassium pump (Na + ,K + -ATPase), and the Na + /K + /2Cl − cotransporter ( Fig. 1 ). The opening of the chloride channels results in the movement of chloride into the intestinal lumen down an electrochemical gradient. Chloride secretion is regulated by a coordinated intracellular and extracellular cascade, involving agonists or antagonists from the intestinal lumen or lamina propria. These agonists or antagonists bind to membrane-bound receptors, for example, vasoactive intestinal polypeptides (VIP) and muscarinic receptors, initiating an intracellular cascade leading to the production of cyclic nucleotides, which enhance chloride secretion. Calcium is another intracellular messenger that binds to calmodulin. This binding creates a complex that increases adenylate cyclase and guanylate cyclase levels, resulting in elevated levels of cAMP and cGMP, which also occurs across intestinal epithelial cells. Calcium-dependent chloride channels, including the Ca 2+ -activated channel proteins, have been described in humans, and in vitro studies suggest that these channels mediate chloride conductance in the human intestine. Further studies show that these channels are regulated by Ca 2+ /calmodulin-dependent protein kinase II, leading to phosphorylation and increased conductance. Inhibition of this kinase has an antidiarrheal effect. Besides inducing chloride secretion, calcium also leads to a decrease in sodium chloride absorption in animal studies. Apical chloride channels have an important role in overall chloride secretion, with the cystic fibrosis transmembrane conductance regulator (CFTR) being the most important. There is evidence to suggest that the interactions between second messenger systems result in greatly enhanced chloride secretion, for example, those activated by cholera toxin.
Epithelial Absorption
Chloride absorption is a passive process and is dependent on concentration gradients and transmural potential differences. Sodium absorption occurs via 3 mechanisms including apical transport proteins: Na + /H + exchange, Na + substrate cotransport, and Na + -PO 4 /Na + -SO 4 cotransport. Sodium and glucose transport by the Na + -glucose cotransporter (SGLT1) occurs by secondary active transport, with sodium gradients, produced by the Na + ,K + -ATPase pump, being the driving force. This process is unaffected by pathologic processes inducing secretion. Chloride secretion is also affected by the proabsorptive neurotransmitters, enkephalins. Enkephalinergic nerves extend to the basolateral membrane of enterocytes, and enkephalins bind to opioid δ receptors, inducing a selective increase in chloride absorption. Water transport across the epithelium has been closely coupled with solute movement.
Intestinal secretion and absorption are also regulated by the peptide hormone, somatostatin. Somatostatin inactivates adenylate cyclase or inhibits calcium influx and potassium efflux. It effectively inhibits the release of gastrointestinal hormones, including secretin, gastrin, cholecystokinin, VIP, motilin, gastric inhibitory polypeptide, and enteroglucagon. The overall effects of this inhibition are reduction in gastric emptying, smooth muscle contractions, level of gastric and pancreatic secretions, and level of chloride secretion by epithelial cells. Both somatostatin and enkephalins are potent intestinal absorbagogues, which have been utilized in the development of diarrheal pharmacotherapy.
Intestinal Secretagogues
Serotonin (5-hydroxytryptamine; 5-HT) and prostaglandin E 2 (PGE 2 ) are potent intestinal secretagogues. Enterochromaffin cells are the main reservoirs of 5-HT. Studies have shown 5-HT to induce fluid secretion from human small intestine and colon. It has a key role in the intestinal secretion induced by cholera toxin, and intraluminal 5-HT concentrations correlate with the magnitude of intestinal secretion. However, Escherichia coli enterotoxins mediate secretion through a 5-HT–independent pathway, confirming the diversity of pathways in the development of diarrheal illnesses. PGE 2 is another potent intestinal secretagogue, with studies showing its administration to cause water and electrolyte secretion. Prostaglandins increase intestinal levels of adenylate cyclase, thereby increasing levels of cAMP, which mediates the secretory effect. The addition of prostaglandins to small intestinal and colonic mucosae mounted in Ussing-type chambers increases short-circuit currents and shifts in sodium and chloride fluxes. Studies in patients with cholera have shown indomethacin (a nonselective cyclooxygenase inhibitor) to reduce fluid secretion. Prostaglandins are integral to the development of diarrhea in inflammatory conditions, with the therapeutic effect attributed to inhibition of PGE 2 synthesis. Relevant neurotransmitter secretagogues include VIP and substance P. VIP is a potent stimulator of cAMP in the intestine and subsequently leads to water and electrolyte secretion in the small intestine. VIP also increases pancreatic bicarbonate secretion and induces smooth muscle relaxation and is thought to be a fundamental part of the secretory neuronal reflex. Patients with neuroendocrine tumors with hypersecretion of VIP experience watery diarrhea, with the initial cases succumbing to dehydration and renal failure. Substance P has been shown to change the net chloride absorption to net secretion. σ-Receptors (opioid σ receptor) are found throughout the central nervous system but their function has been more difficult to characterize. Studies have shown the receptors to be densely expressed in the intestinal mucosa and submucosa of guinea pigs, with a functional role in intestinal motility. More recent studies have proposed that σ-receptors are important in water and electrolyte transport.
Pharmacotherapy
Various cellular pathways have been described earlier and can be used in the development of pharmacotherapy for diarrhea. Although only a limited number of drugs have been evaluated in clinical trials, there are several drugs underdevelopment with future clinical potential.
Drugs Evaluated in Clinical Trials
Oral rehydration therapy
The greatest complication of acute diarrhea is dehydration; therefore, the priority and mainstay of therapy is oral rehydration therapy (ORT). ORT involves the use of glucose-containing fluids, based on the scientific rationale that glucose promotes intestinal ion absorption. SGLT1 cotransports glucose and sodium, closely followed by water, a process that is largely unaffected by pathologic processes. ORT does not reduce the stool volume or duration of illness and, conversely, may increase fecal fluid loss. An attempt to reduce this complication led to the development of hypo-osmolar solutions. Hypo-osmolar ORT in children with persistent diarrhea reduced stool output by approximately 40% and provided a greater resolution of diarrhea compared with standard ORT. Concerns regarding an increased risk of hyponatremia proved to be unfounded. The addition of nonabsorbable starch to ORT reduces fecal fluid loss and shortens the duration of illness in adolescents and adults. This concept is based on the fact that short-chain fatty acids, which are produced in the colon from nonabsorbed carbohydrates, enhance sodium absorption.
Opiates
This class of drugs includes opiates derived from opium, such as morphine or codeine, and synthetic opiates such as loperamide and diphenoxylate. They bind to opioid μ receptors, inducing the secretion of inhibitory neurotransmitter, γ-aminobutyric acid. The result is complex, with increased tone and contraction of intestinal smooth muscles but overall reduced peristaltic activity. The slowed intestinal transit allows increased time for absorption of luminal contents, and constipation is a well-recognized side effect of these medications. It has also been suggested that the antidiarrheal effect of opiates may be due to an antisecretory effect. This suggestion was based on studies showing that morphine and loperamide inhibit chloride secretion in rabbit ileal mucosa and studies in humans showing that loperamide reduced PGE 2 -induced intestinal secretion. However, these findings have not been confirmed by further studies. Morphine crosses the blood-brain barrier, binding to cerebral opioid μ receptors, thereby exerting central effects, including sedation and hypotension. Because of these effects, alongside the risk of morphine dependence, loperamide and diphenoxylate are generally considered for first line treatment, given that they do not cross the blood-brain barrier. Codeine, loperamide, and diphenoxylate are effective in the treatment of chronic diarrhea. Studies have also shown loperamide to increase the maximum basal anal sphincter pressure and the rectal volume required to abolish recovery of the rectoanal inhibitory reflex and to reduce rectal compliance. Consequently, loperamide is effective in the treatment of fecal incontinence, alongside treatment of diarrhea caused by chemotherapy, ileocolic disease or resection, or post-vagotomy, and as an adjunct to antibiotics for traveler’s diarrhea.
Antibiotics
Antibiotics are considered in first line therapy for infectious diarrhea only during specific circumstances. The increasing incidence of antibiotic-resistant infections, treatment side effects, disruption of normal luminal bacterial flora, and the association with complications limit the safety and efficacy of antimicrobial agents. Antibiotics should specifically be avoided in case of E coli 0157 infection because of the association of the antibiotic treatment with the development of hemolytic uremic syndrome. Guidelines suggest situations in which antibiotic treatment is appropriate, which include the following:
- 1.
Traveler’s diarrhea, in which E coli is the likely pathogen, and treatment can shorten the duration of illness
- 2.
Persistent diarrhea, suggestive of giardiasis
- 3.
Febrile diarrheal illnesses consistent with invasive disease
- 4.
Clostridium difficile infection.
Somatostatin
Somatostatin is a potent inhibitor of intestinal secretion and has been used in the development of octreotide, a synthetic analogue with a longer half-life and greater potency than somatostatin. This medication has been most effective in the treatment of neuroendocrine tumors, especially carcinoid tumors, VIPomas, and gastrinomas. However, controlled studies have also shown use of octreotide to be an effective therapy for chemotherapy-induced diarrhea and diarrhea associated with human immunodeficiency virus or AIDS, postgastrectomy dumping syndrome, radiation-induced diarrhea, and short bowel syndrome. Case reports and series have also suggested that somatostatin analogues can be effective for treating diabetic diarrhea, eosinophilic gastroenteritis, graft-versus-host disease, and amyloidosis, although controlled trials are needed to support these clinical applications.
Enkephalinase inhibitors
Enkephalins are endogenous peptides that directly inhibit the production of cAMP by binding to δ-opioid receptors on the enterocyte. The proabsorptive antisecretory potential of enkephalins has been exploited for the pharmacotherapy of diarrhea. Enkephalins are rapidly degraded by the membrane-bound metalloproteinase, enkephalinase, which is found abundantly in the gastrointestinal tract. An inhibitor of enkephalinase, racecadotril (originally known as acetorphan), has been developed for the treatment of acute diarrhea. In vivo studies showed racecadotril to stop cholera toxin-induced secretion, although having no effect on water and electrolyte absorption. Further studies have shown racecadotril to be effective in the treatment of acute diarrhea in adults, with resolution of diarrhea in 92% to 96% of patients. Although efficacy of racecadotril equaled with that of treatment with loperamide, the incidence of reactive constipation was significantly less in the racecadotril group (12.9% vs 29%). Racecadotril has also been effective in treating diarrhea in children, with up to 50% reduction in stool output compared with placebo and also with a reduced duration of illness.
Cholestyramine
The normal enterohepatic circulation of bile salts involves absorption in the distal ileum into the hepatic portal circulation. Diseases that interrupt this process lead to elevated concentrations of bile salts in the colon, where the salts can increase colonic secretion and mucosal permeability and potentially cause mucosal damage. Bile salt malabsorption can be idiopathic; caused by ileal resection, Crohn disease, radiation enteritis, and bacterial overgrowth; or may occur postcholecystectomy. Cholestyramine is a nonabsorbable anion exchanger that binds and neutralizes bile salts, and studies have shown cholestyramine to be an effective antidiarrheal agent for bile salt diarrhea.
5-HT antagonists
5-HT is an obvious pharmacologic target, but studies in humans investigating 5-HT antagonists have produced conflicting results. Antagonists to 5-HT 2 , 5-HT 3 , and 5-HT 4 receptors can markedly reduce or reverse the cholera toxin–induced secretory state. However, this effect is generally observed only when antagonists are given before exposure to the toxin rather than during the illness. More significantly, when used in humans, the 5-HT 3 antagonist, alosetron, was associated with ischemic colitis and is therefore only available with a restricted label for safety reasons. Cilansetron has been withdrawn from the market.
Calcium-calmodulin antagonists
Calmodulin is involved in calcium-dependent chloride secretion and is a natural target for the development of antidiarrheal medicines. Calmodulin binding has an antidiarrheal effect. Studies that first exploited this pathway used chlorpromazine, a phenothiazine that inhibits calmodulin, adenylate cyclase, and cAMP. Chlorpromazine reduced the duration of diarrhea, frequency of vomiting, and the amount of intravenous fluid required. However, its use is limited by its α-adrenergic receptor–blocking activity, resulting in hypotension and sedation. Zaldaride maleate, a calmodulin antagonist, is an effective antidiarrheal agent but has no superiority over loperamide. As a result, further development in these agents was discontinued, especially given the incidence of cardiovascular effects when used at high doses.
Bismuth
Traditionally, bismuth has been used in the treatment of dyspepsia. However, it has also been shown to act as an antidiarrheal agent due to its antisecretory, antiinflammatory, and antimicrobial properties. Bismuth is most effective in the prevention of traveler’s diarrhea, more specifically by reducing the incidence of enterotoxigenic E coli . A study showed bismuth to be an effective agent in the treatment of irritable bowel syndrome and microscopic colitis.
Berberine
Berberine is a plant alkaloid with a long history of medicinal use in Chinese and Ayurvedic medicine. It has been shown to have in vitro activity against viruses, parasites, and bacteria. This antimicrobial activity has been translated into the clinical setting, with trials showing berberine to reduce stool volume and stop diarrhea more effectively than placebo in cases of enterotoxigenic E coli . There has also been a single pilot placebo-controlled study investigating the use of berberine in patients undergoing abdominal radiotherapy. Berberine significantly reduced the incidence and severity of radiation-induced acute intestinal symptoms (RIAIS) and delayed the occurrence of RIAIS in patients undergoing abdominal or whole pelvic radiotherapy.
Drugs Underdevelopment
Chloride channel antagonists
The chloride channel, CFTR, is a crucial factor in the intestinal secretory process, and research has been directed at the potential of using CFTR as a pharmacologic target. In vitro studies have shown sulfonylureas (glibenclamide ) and nonsulfonylurea hypoglycemic drugs to block the CFTR channel and inhibit chloride currents. Disulfonic stilbenes and arylaminobenzoates also block the CFTR, but in vitro studies have shown these compounds, as well as sulfonylureas, to be nonspecific, working at several cellular sites that may indirectly alter the CFTR. Glycine hydrazide and thiazolidinone CFTR inhibitors reduce intestinal fluid losses in animal models of cholera toxin–mediated secretory diarrhea. The thiazolidinedione drugs, rosiglitazone and pioglitazone, are peroxisome proliferator-activated receptor γ agonists, which are in widespread clinical use as insulin-sensitizing agents in type 2 diabetes. These drugs reduced cholera toxin–induced intestinal fluid accumulation by 65% in mouse intestinal segments, and these changes were partly attributed to a reduced expression of the CFTR-chloride channel. Traditional antidiarrheal remedies, including cocoa beans, bark latex of the tree Croton lechleri (Euphorbiaceae; “sangre de drago”), boiled rice (or more specifically an unidentified rice factor), and hydrolyzable tannin extracted from Chinese gallnut, exert their effect through inhibition of the CFTR channel. Despite in vitro and animal studies suggesting a role for CFTR inhibition in the treatment of diarrhea, the only study in humans investigating CFTR inhibition was with SP-303, a novel investigatory agent derived from C lechleri . A placebo-controlled trial showed SP-303 to reduce the duration of traveler’s diarrhea by 21%.
σ-Receptor agonists
The function of the σ-receptor has not yet been clearly defined, with the activation of the receptor leading to a variety of physiologic changes, including tachycardia, mydriasis, hypertonia, tachypnea, as well as psychotropic effects such as anti-depressive actions, euphoria, malaise, and anxiety. However, σ-receptor ligands have also been shown to have an antisecretory role in animal studies of bacteria-induced secretory diarrhea. A small study investigating igmesine, a σ-receptor ligand, in PGE 2 -induced intestinal secretion, showed igmesine to inhibit secretion in humans.
VIP antagonists
VIP is a potent intestinal secretagogue, and a study on VIP antagonists has confirmed the role of VIP in fluid and electrolyte secretion induced by heat-labile toxins of cholera and E coli . In cholera toxin–induced secretion in the rat jejunum, the VIP antagonist, [4Cl- D -Phe6, Leu17]-VIP, reduced intestinal secretion to normal levels. Ultimately, VIP antagonists can inhibit the secretory responses to electric stimulation of mucosal neurons and effectively attenuate the secretory response both before and after luminal application of cholera and E coli enterotoxins. The use of VIP antagonists has not yet been studied in humans.
Substance P antagonists
Animal studies have shown substance P antagonists to reduce electrolyte and water secretion caused by cholera toxin and C difficile toxin A but not by E coli enterotoxin. The exact role of substance P in the development of diarrhea has not been clarified, and consequently, the importance of substance P antagonists in human disease is unknown. Studies have not been performed in humans, and it is unlikely these antagonists will have a major role as antidiarrheal agents.
Pharmacotherapy
Various cellular pathways have been described earlier and can be used in the development of pharmacotherapy for diarrhea. Although only a limited number of drugs have been evaluated in clinical trials, there are several drugs underdevelopment with future clinical potential.
Drugs Evaluated in Clinical Trials
Oral rehydration therapy
The greatest complication of acute diarrhea is dehydration; therefore, the priority and mainstay of therapy is oral rehydration therapy (ORT). ORT involves the use of glucose-containing fluids, based on the scientific rationale that glucose promotes intestinal ion absorption. SGLT1 cotransports glucose and sodium, closely followed by water, a process that is largely unaffected by pathologic processes. ORT does not reduce the stool volume or duration of illness and, conversely, may increase fecal fluid loss. An attempt to reduce this complication led to the development of hypo-osmolar solutions. Hypo-osmolar ORT in children with persistent diarrhea reduced stool output by approximately 40% and provided a greater resolution of diarrhea compared with standard ORT. Concerns regarding an increased risk of hyponatremia proved to be unfounded. The addition of nonabsorbable starch to ORT reduces fecal fluid loss and shortens the duration of illness in adolescents and adults. This concept is based on the fact that short-chain fatty acids, which are produced in the colon from nonabsorbed carbohydrates, enhance sodium absorption.
Opiates
This class of drugs includes opiates derived from opium, such as morphine or codeine, and synthetic opiates such as loperamide and diphenoxylate. They bind to opioid μ receptors, inducing the secretion of inhibitory neurotransmitter, γ-aminobutyric acid. The result is complex, with increased tone and contraction of intestinal smooth muscles but overall reduced peristaltic activity. The slowed intestinal transit allows increased time for absorption of luminal contents, and constipation is a well-recognized side effect of these medications. It has also been suggested that the antidiarrheal effect of opiates may be due to an antisecretory effect. This suggestion was based on studies showing that morphine and loperamide inhibit chloride secretion in rabbit ileal mucosa and studies in humans showing that loperamide reduced PGE 2 -induced intestinal secretion. However, these findings have not been confirmed by further studies. Morphine crosses the blood-brain barrier, binding to cerebral opioid μ receptors, thereby exerting central effects, including sedation and hypotension. Because of these effects, alongside the risk of morphine dependence, loperamide and diphenoxylate are generally considered for first line treatment, given that they do not cross the blood-brain barrier. Codeine, loperamide, and diphenoxylate are effective in the treatment of chronic diarrhea. Studies have also shown loperamide to increase the maximum basal anal sphincter pressure and the rectal volume required to abolish recovery of the rectoanal inhibitory reflex and to reduce rectal compliance. Consequently, loperamide is effective in the treatment of fecal incontinence, alongside treatment of diarrhea caused by chemotherapy, ileocolic disease or resection, or post-vagotomy, and as an adjunct to antibiotics for traveler’s diarrhea.
Antibiotics
Antibiotics are considered in first line therapy for infectious diarrhea only during specific circumstances. The increasing incidence of antibiotic-resistant infections, treatment side effects, disruption of normal luminal bacterial flora, and the association with complications limit the safety and efficacy of antimicrobial agents. Antibiotics should specifically be avoided in case of E coli 0157 infection because of the association of the antibiotic treatment with the development of hemolytic uremic syndrome. Guidelines suggest situations in which antibiotic treatment is appropriate, which include the following:
- 1.
Traveler’s diarrhea, in which E coli is the likely pathogen, and treatment can shorten the duration of illness
- 2.
Persistent diarrhea, suggestive of giardiasis
- 3.
Febrile diarrheal illnesses consistent with invasive disease
- 4.
Clostridium difficile infection.
Somatostatin
Somatostatin is a potent inhibitor of intestinal secretion and has been used in the development of octreotide, a synthetic analogue with a longer half-life and greater potency than somatostatin. This medication has been most effective in the treatment of neuroendocrine tumors, especially carcinoid tumors, VIPomas, and gastrinomas. However, controlled studies have also shown use of octreotide to be an effective therapy for chemotherapy-induced diarrhea and diarrhea associated with human immunodeficiency virus or AIDS, postgastrectomy dumping syndrome, radiation-induced diarrhea, and short bowel syndrome. Case reports and series have also suggested that somatostatin analogues can be effective for treating diabetic diarrhea, eosinophilic gastroenteritis, graft-versus-host disease, and amyloidosis, although controlled trials are needed to support these clinical applications.
Enkephalinase inhibitors
Enkephalins are endogenous peptides that directly inhibit the production of cAMP by binding to δ-opioid receptors on the enterocyte. The proabsorptive antisecretory potential of enkephalins has been exploited for the pharmacotherapy of diarrhea. Enkephalins are rapidly degraded by the membrane-bound metalloproteinase, enkephalinase, which is found abundantly in the gastrointestinal tract. An inhibitor of enkephalinase, racecadotril (originally known as acetorphan), has been developed for the treatment of acute diarrhea. In vivo studies showed racecadotril to stop cholera toxin-induced secretion, although having no effect on water and electrolyte absorption. Further studies have shown racecadotril to be effective in the treatment of acute diarrhea in adults, with resolution of diarrhea in 92% to 96% of patients. Although efficacy of racecadotril equaled with that of treatment with loperamide, the incidence of reactive constipation was significantly less in the racecadotril group (12.9% vs 29%). Racecadotril has also been effective in treating diarrhea in children, with up to 50% reduction in stool output compared with placebo and also with a reduced duration of illness.
Cholestyramine
The normal enterohepatic circulation of bile salts involves absorption in the distal ileum into the hepatic portal circulation. Diseases that interrupt this process lead to elevated concentrations of bile salts in the colon, where the salts can increase colonic secretion and mucosal permeability and potentially cause mucosal damage. Bile salt malabsorption can be idiopathic; caused by ileal resection, Crohn disease, radiation enteritis, and bacterial overgrowth; or may occur postcholecystectomy. Cholestyramine is a nonabsorbable anion exchanger that binds and neutralizes bile salts, and studies have shown cholestyramine to be an effective antidiarrheal agent for bile salt diarrhea.
5-HT antagonists
5-HT is an obvious pharmacologic target, but studies in humans investigating 5-HT antagonists have produced conflicting results. Antagonists to 5-HT 2 , 5-HT 3 , and 5-HT 4 receptors can markedly reduce or reverse the cholera toxin–induced secretory state. However, this effect is generally observed only when antagonists are given before exposure to the toxin rather than during the illness. More significantly, when used in humans, the 5-HT 3 antagonist, alosetron, was associated with ischemic colitis and is therefore only available with a restricted label for safety reasons. Cilansetron has been withdrawn from the market.
Calcium-calmodulin antagonists
Calmodulin is involved in calcium-dependent chloride secretion and is a natural target for the development of antidiarrheal medicines. Calmodulin binding has an antidiarrheal effect. Studies that first exploited this pathway used chlorpromazine, a phenothiazine that inhibits calmodulin, adenylate cyclase, and cAMP. Chlorpromazine reduced the duration of diarrhea, frequency of vomiting, and the amount of intravenous fluid required. However, its use is limited by its α-adrenergic receptor–blocking activity, resulting in hypotension and sedation. Zaldaride maleate, a calmodulin antagonist, is an effective antidiarrheal agent but has no superiority over loperamide. As a result, further development in these agents was discontinued, especially given the incidence of cardiovascular effects when used at high doses.
Bismuth
Traditionally, bismuth has been used in the treatment of dyspepsia. However, it has also been shown to act as an antidiarrheal agent due to its antisecretory, antiinflammatory, and antimicrobial properties. Bismuth is most effective in the prevention of traveler’s diarrhea, more specifically by reducing the incidence of enterotoxigenic E coli . A study showed bismuth to be an effective agent in the treatment of irritable bowel syndrome and microscopic colitis.
Berberine
Berberine is a plant alkaloid with a long history of medicinal use in Chinese and Ayurvedic medicine. It has been shown to have in vitro activity against viruses, parasites, and bacteria. This antimicrobial activity has been translated into the clinical setting, with trials showing berberine to reduce stool volume and stop diarrhea more effectively than placebo in cases of enterotoxigenic E coli . There has also been a single pilot placebo-controlled study investigating the use of berberine in patients undergoing abdominal radiotherapy. Berberine significantly reduced the incidence and severity of radiation-induced acute intestinal symptoms (RIAIS) and delayed the occurrence of RIAIS in patients undergoing abdominal or whole pelvic radiotherapy.
Drugs Underdevelopment
Chloride channel antagonists
The chloride channel, CFTR, is a crucial factor in the intestinal secretory process, and research has been directed at the potential of using CFTR as a pharmacologic target. In vitro studies have shown sulfonylureas (glibenclamide ) and nonsulfonylurea hypoglycemic drugs to block the CFTR channel and inhibit chloride currents. Disulfonic stilbenes and arylaminobenzoates also block the CFTR, but in vitro studies have shown these compounds, as well as sulfonylureas, to be nonspecific, working at several cellular sites that may indirectly alter the CFTR. Glycine hydrazide and thiazolidinone CFTR inhibitors reduce intestinal fluid losses in animal models of cholera toxin–mediated secretory diarrhea. The thiazolidinedione drugs, rosiglitazone and pioglitazone, are peroxisome proliferator-activated receptor γ agonists, which are in widespread clinical use as insulin-sensitizing agents in type 2 diabetes. These drugs reduced cholera toxin–induced intestinal fluid accumulation by 65% in mouse intestinal segments, and these changes were partly attributed to a reduced expression of the CFTR-chloride channel. Traditional antidiarrheal remedies, including cocoa beans, bark latex of the tree Croton lechleri (Euphorbiaceae; “sangre de drago”), boiled rice (or more specifically an unidentified rice factor), and hydrolyzable tannin extracted from Chinese gallnut, exert their effect through inhibition of the CFTR channel. Despite in vitro and animal studies suggesting a role for CFTR inhibition in the treatment of diarrhea, the only study in humans investigating CFTR inhibition was with SP-303, a novel investigatory agent derived from C lechleri . A placebo-controlled trial showed SP-303 to reduce the duration of traveler’s diarrhea by 21%.
σ-Receptor agonists
The function of the σ-receptor has not yet been clearly defined, with the activation of the receptor leading to a variety of physiologic changes, including tachycardia, mydriasis, hypertonia, tachypnea, as well as psychotropic effects such as anti-depressive actions, euphoria, malaise, and anxiety. However, σ-receptor ligands have also been shown to have an antisecretory role in animal studies of bacteria-induced secretory diarrhea. A small study investigating igmesine, a σ-receptor ligand, in PGE 2 -induced intestinal secretion, showed igmesine to inhibit secretion in humans.
VIP antagonists
VIP is a potent intestinal secretagogue, and a study on VIP antagonists has confirmed the role of VIP in fluid and electrolyte secretion induced by heat-labile toxins of cholera and E coli . In cholera toxin–induced secretion in the rat jejunum, the VIP antagonist, [4Cl- D -Phe6, Leu17]-VIP, reduced intestinal secretion to normal levels. Ultimately, VIP antagonists can inhibit the secretory responses to electric stimulation of mucosal neurons and effectively attenuate the secretory response both before and after luminal application of cholera and E coli enterotoxins. The use of VIP antagonists has not yet been studied in humans.
Substance P antagonists
Animal studies have shown substance P antagonists to reduce electrolyte and water secretion caused by cholera toxin and C difficile toxin A but not by E coli enterotoxin. The exact role of substance P in the development of diarrhea has not been clarified, and consequently, the importance of substance P antagonists in human disease is unknown. Studies have not been performed in humans, and it is unlikely these antagonists will have a major role as antidiarrheal agents.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







