The commonly used regimens for the eradication of Helicobacter pylori infection consist of administration of proton pump inhibitors (PPIs) and 1 to 3 antimicrobial agents, such as amoxicillin, clarithromycin, metronidazole, fluoroquinolone, or tetracycline. Each agent has its own pharmacologic characteristics. PPIs are metabolized by cytochrome P450 2C19 (CYP2C19), which is polymorphic. CYP2C19 genotypic differences in the pharmacokinetics and pharmacodynamics of PPIs influence the eradication rates of H pylori infection by PPI-containing regimens. Amoxicillin is a time-dependent antibiotic, whereas clarithromycin, metronidazole, tetracycline, and fluoroquinolone are not. The plasma half-life of antimicrobial agents also differs among these antibiotics. To achieve consistently high eradication rates, the eradication regimens must be designed based on a good understanding of the resistance patterns of the bacteria and the pharmacologic characteristics of the agents used for H pylori eradication therapy.
A close relationship has been found between Helicobacter pylori infection and upper gastrointestinal disorders such as peptic ulcer diseases, gastric cancer, and gastric mucosa–associated lymphoid tissue lymphoma. Eradication of H pylori is a part of the effective treatment and/or prevention of these disorders and also reduces the occurrence of new gastric cancers after endoscopic resection. At present, the most common methods for the eradication of H pylori infection consist of the administration of a proton pump inhibitor (PPI) and antimicrobial agents, such as amoxicillin, clarithromycin, metronidazole, fluoroquinolone, or tetracycline. Each of these agents has its own characteristics in respect to pharmacokinetics, pharmacodynamics, and pharmacogenomics, which theoretically affect treatment success attained with the different therapeutic regimens. This article describes the pharmacologic characteristics of the common agents used for eradication of H pylori infection. This knowledge should be helpful for clinicians trying to achieve optimal eradication of H pylori infection and investigators designing new treatment protocols.
Pharmacologic characteristics of representative therapeutic agents involved in regimens for eradication of H pylori infection
Proton Pump Inhibitor
PPIs potentially play a major role in an H pylori eradication therapy by (1) increasing the intragastric pH, which improves antibiotic stability and bioavailability ; (2) increasing the intragastric pH to 6 or more, which prompts H pylori to replicate and thus become more sensitive to antibiotics that are effective only against replicating bacteria, such as amoxicillin ; (3) suppressing acid secretion, which increases the concentration of antibiotics in the stomach ; and (4) having an anti- H pylori effect.
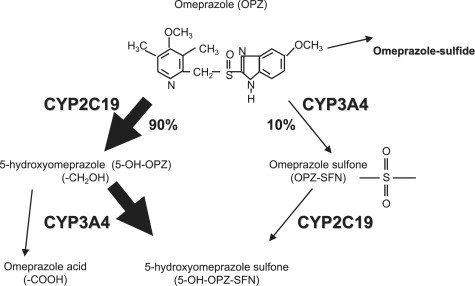
PPIs are primarily metabolized by cytochrome P450 (CYP) 2C19 (CYP2C19) ( Fig. 1 ). The genetic polymorphisms of CYP2C19 are classified into 3 groups: rapid metabolizer (RM: *1/*1), intermediate metabolizer (IM: *1/*X), and poor metabolizer (PM: *X/*X), (*1 = wild type allele and *X = mutated allele). Recently, the CYP 2C 19*17 allele has been found in the ultrarapid extensive metabolizer genotype of CYP2C19. However, the clinical effect of CYP 2C 19*17 remains to be elucidated.
Although various genetic mutations involved in the CYP2C19 polymorphisms have been discovered from different ethnic populations, the differences in the activity of CYP2C19 can be explained in most cases by the combination of 2 point mutations, CYP2C19*2 of exon 5 and CYP2C19*3 of exon 4. There are interethnic differences in the frequencies of PM genotypes of this enzyme. Representative frequencies of phenotypes and alleles in different ethnic groups are summarized in Table 1 .
| Ethnicity | Phenotype Frequency | Allele Frequency | References | ||||
|---|---|---|---|---|---|---|---|
| RM | IM | PM | *1 | *2 | *3 | ||
| Africans | 0.68 | 0.28 | 0.04 | 0.823 | 0.173 | 0.004 | |
| Asians | 0.35 | 0.46 | 0.19 | 0.58 | 0.29 | 0.13 | |
| Caucasians | 0.69 | 0.28 | 0.03 | 0.83 | 0.17 | 0 | |
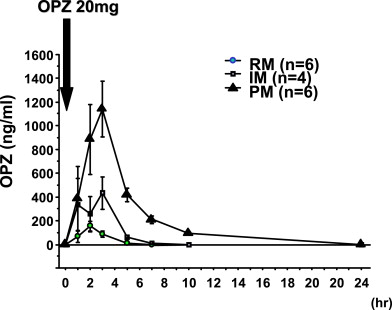
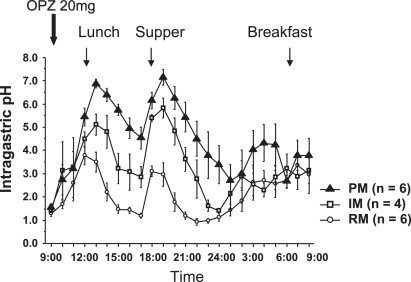
When omeprazole, 20 mg, is given as a single dose, plasma omeprazole concentrations differ among the 3 different CYP2C19 genotypic groups (RM, IM, and PM) ( Fig. 2 ). Plasma omeprazole levels in the PM group are sustained for a longer time after dosing. The pharmacokinetic data in relation to CYP2C19 genotypes are summarized in Table 2 . When a PPI (ie, omeprazole, 20 mg) is administered, the intragastric pH profile also differs among the 3 different genotypic groups ( Fig. 3 ). The mean 24-hour intragastric pH of the RM group is the lowest, the IM group comes next, and the PM group is the highest. Several reports on intragastric pH profiles after PPI dosing are summarized in Table 3 . The differences in acid inhibition by a PPI among the different CYP2C19 genotypic groups are considered to result from the different plasma concentrations of the PPI among the different genotypic groups.
| Regimen | RM | IM | PM | RM/IM/PM ratio | References |
|---|---|---|---|---|---|
| OPZ, 20 mg, day 1 | 421 | 1403 | 5109 | 1:3.3:12.2 | |
| OPZ, 20 mg, day 1 | 524 | 1096 | 5607 | 1:2.1:10.7 | |
| OPZ, 20 mg, day 8 | 1057 | 2418 | 7153 | 1:2.3:6.8 | |
| RPZ, 20 g, day 1 | 696 | 1609 | 2329 | 1:2.3:3.3 | |
| RPZ, 20 mg, day 8 | 464 | 1398 | 2437 | 1:3.0:5.3 | |
| LPZ, 30 mg, day 8 | 1980 | 4775 | 10,663 | 1:2.4:5.4 |
| Regimen | RM | IM | PM | References |
|---|---|---|---|---|
| OPZ, 20 mg, day 1 | 2.1 | 3.3 | 4.5 | |
| OPZ, 20 mg, day 1 | 2.3 | 3.3 | 4.1 | |
| OPZ, 20 mg, day 8 | 4.1 | 4.7 | 5.9 | |
| LPZ, 30 mg, day 8 | 4.4 | 4.9 | 5.4 | |
| RPZ, 20 mg, day 1 | 3.3 | 4.2 | 5.3 | |
| RPZ, 20 mg, day 8 | 4.8 | 5.0 | 6.0 |
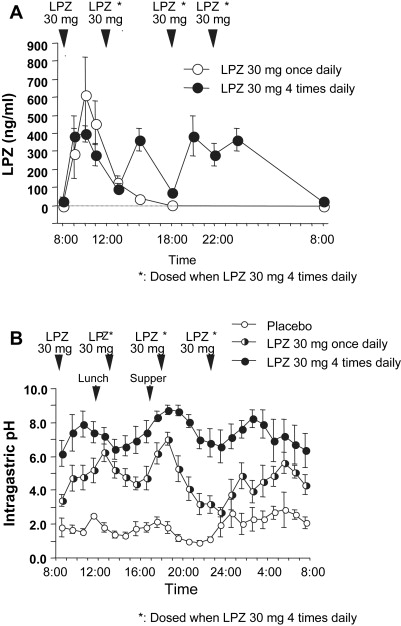
When lansoprazole, 30 mg, is given 4 times daily to sustain the plasma lansoprazole levels all day long ( Fig. 4 A), near-complete acid inhibition can be achieved, even among the RM genotypes (see Fig. 4 B). The peak plasma concentration (Cmax) of lansoprazole is not increased in the RM group with lansoprazole, 30 mg, given 4 times daily when compared with that of once daily administration of lansoprazole, 30 mg, (see Fig. 4 A) and is not as high as that observed in the PM group. Therefore, the dosing regimen of a PPI is a key element when attempting to attain sustained levels of high intragastric pH. Clinically, one would wish to be able to estimate the effectiveness of a PPI dosing regimen irrespective of the CYP2C19 genotype (see later discussion).
Amoxicillin
Amoxicillin is a penicillin derivative that inhibits the synthesis of the bacterial cell wall. Therefore, amoxicillin’s bactericidal effect requires the bacteria to be replicating.
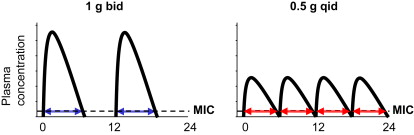
Amoxicillin is excreted by the kidneys, the plasma half-life is approximately 1 hour, and the bactericidal effect is time dependent. Moreover, amoxicillin has little postantibiotic effect (PAE) on gram-negative bacteria, such as H pylori . Therefore, theoretically, amoxicillin should be given 3 or 4 times daily to maximize the time above minimal inhibitory concentration (MIC) ( Fig. 5 ). However, in most H pylori eradication therapies, amoxicillin is given twice daily, where the estimated time above MIC attained by twice daily dosing is insufficient for amoxicillin. Therefore, if a patient infected with clarithromycin-resistant strain of H pylori is treated with triple therapy with PPI/amoxicillin/clarithromycin twice daily, the chance of eradication of H pylori infection is low.
Amoxicillin is also somewhat acid labile, and both its stability and bioavailability in the stomach are improved by the concomitant use of a PPI. Because most strains of H pylori are sensitive to amoxicillin and the drug is given 3 or 4 times daily with appropriate dosing of a PPI to attain sufficient acid inhibition, high eradication rates can been achieved with dual PPI/amoxicillin therapy as discussed later.
Clarithromycin
Clarithromycin is a macrolide and often included in the standard regimens for the eradication of H pylori infection. The plasma half-life of clarithromycin is relatively long (around 5 hours), such that a twice daily dosing is an appropriate dosing schedule. The prevalence of clarithromycin-resistant H pylori strains is increasing all over the world, and this increase has resulted in a decrease in the eradication rates with clarithromycin-containing regimens, such as the combination of PPI/amoxicillin/clarithromycin. Bacterial resistance to clarithromycin can be estimated by the measurement of point mutations of the 23S ribosomal RNA (rRNA) gene at positions 2142 and 2143.
Clarithromycin is a strong inhibitor of CYP3A4. Therefore, clinicians must pay attention to the risk of drug-drug interactions in patients who are treated with other drugs that are metabolized by the CYP3A4 pathway. Plasma levels of a PPI are also increased by clarithromycin, which also inhibits P-glycoprotein (MDR1), resulting in the increased risk of adverse events with drugs that are also substrates of MDR1, such as digoxin.
Metronidazole
Metronidazole has been used widely for the eradication of H pylori infection together with amoxicillin or clarithromycin and a PPI. The bactericidal mechanism of metronidazole is unique. Metronidazole is a prodrug, and the nitro moiety of metronidazole is reduced by bacteria, which induces DNA double-strand breaks resulting in cell death. The plasma half-life of metronidazole is around 8 hours. Therefore, a twice or thrice daily dosing is appropriate.
There are marked geographic differences in the distribution of metronidazole-resistant strains of H pylori . Resistance to metronidazole is associated with decreased eradication rates when metronidazole-based regimens are used. However, metronidazole is unique among the commonly used antibiotics because resistance to this drug can be partially overcome by increasing the dose and duration of therapy.
Metronidazole also inhibits CYP3A4 and CYP2C9. Therefore, clinicians should pay attention to drug-drug interactions with substrates of CYP3A4 and CYP2C9, such as warfarin, when metronidazole is given. Metronidazole also inhibits aldehyde dehydrogenase in the metabolic process of alcohol breakdown, resulting in an increase in blood acetaldehyde levels and thus can cause a disulfiram (Antabuse)-like reaction. Patients are advised not to drink alcohol while taking metronidazole or the similar nitroimidazole, tinidazole.
Fluoroquinolones
Fluoroquinolones, such as levofloxacin, are now used for eradication of H pylori infection. Fluoroquinolones disturb the function of gyrase in bacteria, which is an essential enzyme for DNA replication, resulting in the induction of DNA breaks and cell death. Fluoroquinolone-containing regimens are often used in rescue regimens after failure of standard regimens. However, the worldwide overuse of fluoroquinolones has led to a rapid increase in resistance such that it is unlikely that this group of drug will be a useful anti- H pylori agent without prior susceptibility testing.
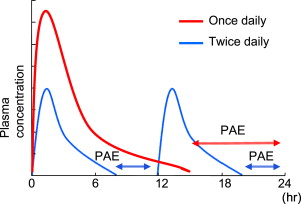
The bactericidal effect of fluoroquinolones depends on the Cmax and the area under the curve and not on the time above MIC. Fluoroquinolones have PAE, the duration of which depends on Cmax. Therefore, a higher dose of the fluoroquinolone given once daily is the best dosing scheme ( Fig. 6 ). Di Caro and colleagues reported that levofloxacin, 500 mg once daily, was as effective as levofloxacin, 500 mg twice daily, when used with amoxicillin and esomeprazole. Therefore, the authors suggest that fluoroquinolones should be dosed once daily at a higher dose.
Tetracycline/Minocycline
Tetracycline antibiotics (eg, tetracycline and minocycline) bind to the bacterial 70S rRNA and disturb the aminoacyl transfer RNA from combining with the messenger RNA and ribosome composite, resulting in the inhibition of protein synthesis. Tetracycline was involved in the classical triple therapy with bismuth subcitrate and tinidazole. The incidence of tetracycline-resistant strains of H pylori is very low in most countries. The plasma half-life of tetracycline is around 6 hours, and therefore, twice daily dosing is theoretically an appropriate dosing scheme for tetracycline. However, the most studied tetracycline-containing regimen (tetracycline hydrochloride, metronidazole, bismuth, and a PPI) used tetracycline, 500 mg, 4 times a day. This regimen has not been adequately tested in a head-to-head comparison with twice-a-day tetracycline regimens. Such studies are clearly needed.
Combinations of Antimicrobial Agents for Regimens Used in Eradication of H pylori Infection
In the most effective eradication regimens, 2 or 3 antimicrobial agents are used. However, clinicians must pay attention to the combination of antimicrobial agents. When amoxicillin is taken together with tetracycline, the latter may theoretically decrease the ability of amoxicillin to kill bacteria.
Both clarithromycin and levofloxacin have effects on cardiac electric signaling. When clarithromycin and levofloxacin are used together, the effect of either drug on the heart may be increased or prolonged, resulting in the alteration of cardiac rhythm, which may be dangerous or potentially life threatening.
On the positive side, metronidazole has an additional or a synergistic bactericidal effect on the eradication of H pylori infection with any of the antimicrobial agents mentioned earlier.
Therefore, commonly used regimens for the eradication of H pylori infection include (1) amoxicillin and clarithromycin, (2) amoxicillin and metronidazole, (3) amoxicillin and a fluoroquinolone, (4) clarithromycin and metronidazole, (5) a fluoroquinolone and metronidazole, and (6) tetracycline and metronidazole. These combinations of antimicrobial agents are administered with a PPI. The combination of clarithromycin and tetracycline was also reported to achieve a high eradication rate. There have been few studies on the combinations of tetracycline and fluoroquinolones.
Sequential therapy (PPI/amoxicillin followed by PPI/metronidazole/clarithromycin) has been found to achieve sufficient eradication rates. However, concomitant therapy with a PPI, amoxicillin, metronidazole, and clarithromycin has also been found to achieve the high eradication rates attained by sequential therapy.
Pharmacogenetics in H pylori eradication therapy
CYP2C19 Genotypic Status as the Therapeutic Determinant of PPI-Containing Eradication Therapy for H pylori Infection
The first report on the influence of CYP2C19 polymorphisms on H pylori eradication rates was with the dual PPI/amoxicillin therapy. The eradication rates for H pylori infection by dual therapy with omeprazole, 20 mg once daily, and amoxicillin, 500 mg 4 times daily, for 2 weeks are around 30% in those with the RM genotype, 60% in those with IM genotype, and 100% in those with PM genotype (see Table 3 ). Differences in plasma omeprazole levels among the different CYP2C19 genotypic groups are assumed to reflect the different eradication rates among the correspondent genotypic groups. Other reports on the influences of dual PPI/amoxicillin therapy are summarized in Table 4 .








