Peyronie disease (PD) is an incurable, sexually debilitating disease resulting in penile deformity, coital failure, and significant psychological stress for patients and their partners. Appropriate treatment should be individualized and tailored to the patient’s goals and expectations, disease history, physical examination findings, and erectile function. After medical therapy is considered and the disease has stabilized, surgical correction, including tunical shortening or lengthening procedures, is an excellent option for patients with functional impairment caused by PD. Outcomes are satisfactory when proper treatment decisions are made, with the goal being expected return to normal sexual function following PD treatment.
Peyronie disease (PD) is an incurable, fibrotic disease of the tunica albuginea, which causes penile curvature with a loss of coital function in many patients. Scar-like plaques form between layers of the thick fibroelastic tunica, and currently experts hypothesize that the plaques occur as a result of abnormal wound healing in response to repeated microtrauma and/or more obvious traumatic buckling of the rigid phallus. The reported prevalence of PD ranges from 3.2% to 8.9%, with a mean age of 57.4 years and an incidence that clearly increases with aging. Clinically the plaques present with penile curvature, hour-glass deformity, and/or erectile dysfunction (ED) often caused by venoocclusive incompetence, or they may be asymptomatic. Presentation can also include penile pain with erection, inability to have intercourse secondary to penile deformity, and a palpable plaque.
The natural history of PD includes both an active and quiescent phase of the disease. The active, or inflammatory, portion of the disease state is characterized by painful erections, an evolving plaque, and progressive development of penile curvature, and usually lasts 12 to 24 months from the time of onset. Studies have shown that almost all men (94%) will experience resolution of coital pain within 18 months. The quiescent phase is characterized by stability of the penile deformity, resolution of penile pain, and in some, the onset of ED. Both early and more current reports have confirmed that without treatment only 12% to 13% of men will improve, roughly 40% to 48% will worsen, and 40% to 47% will maintain a stable deformity. Given these findings, along with the well-documented psychosocial implications of the disease, men for hundreds of years have sought treatment for this debilitating condition.
Ultimately, treatment is designed to improve coital function and result in a satisfactory, comfortable erection for both patient and partner. Most patients prefer nonsurgical intervention before proceeding with a surgical procedure. Nonsurgical therapies have included: expectorant, oral medications, intralesional injections, extracorporeal shock-wave therapy, and ultrasound. Treatment efforts began with de la Peyronie’s original recommendation to bathe in the warm waters of Barèges in southern France. Unfortunately, despite the multitude of modalities that have been tried, current medical therapies have offered limited success in producing tangible results for patients.
Surgery for Peyronie disease
Surgery is recommended for patients with stable PD and poor coital function. This poor function may result from the penile curvature, from hourglass deformity resulting in distal flaccidity, or from ED caused by the PD plaque or venoocclusive dysfunction. Surgery is usually avoided during the active phase of the disease, and this provides an opportunity for patients to pursue medical therapies. Montorsi and colleagues recommend waiting at least 12 months from the end of the active phase of PD before considering surgery, suggesting in fact that if surgery is undertaken in men with stable disease of less than 6 months’ duration, many will suffer from postoperative recurrence.
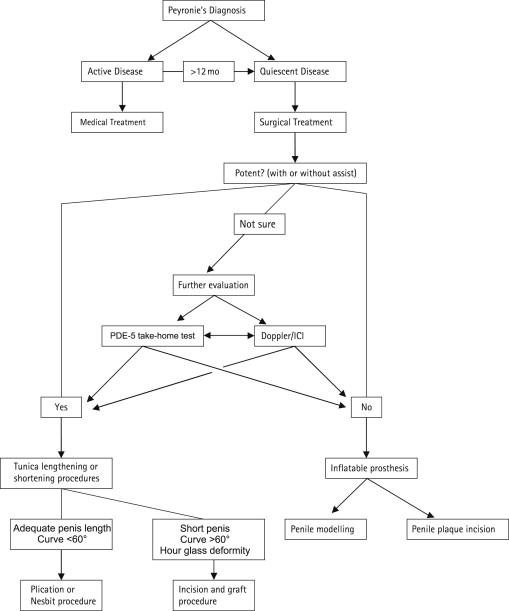
The choice of a surgical procedure depends on each patient’s needs and preferences. Counseling and decision making should be based on the patient’s current coital function as reported in their history, their deformity on physical examination, and their erectile rigidity. Three surgical categories are used for PD patients ( Fig. 1 ), and the evaluation process must identify which surgery will best serve each unique patient. Corporoplasty or plication techniques generally have the best outcomes regarding postoperative sexual satisfaction and erectile function, and are the least invasive approach, but are reserved for patients with adequate erections, simple curvature of 60° or less, and adequate penile length to undergo the additional shortening that may occur with the procedure. Plaque incision/excision and grafting procedures are used for more severe or complex curves, hourglass deformities, and in men who have already suffered significant penile shortening secondary to PD, as these procedures will lengthen the tunica. Inflatable penile prosthesis (IPP) implantation is reserved for men with PD and refractory ED, or men who prefer this method of treatment. Men with satisfactory erectile function with or without supportive medications are candidates for straightening procedures using either tunical lengthening or shortening operations.
Evaluation of patients for surgery
Key factors in evaluating patients for proper placement in the surgical treatment algorithm are degree and complexity of curve, baseline penile length and percent of estimated loss of length with correction, and baseline erectile function. All of these factors are easily evaluated, mostly through physical examination, with the exception of baseline erectile function.
Determining a patient’s baseline erectile status is of prime importance in selecting the surgical treatment that will lead to a satisfactory outcome. Potency may be evaluated by sexual history, a phosphodiesterase-5 (PDE-5) inhibitor take-home test, or intercavernosal injection (ICI) ± Doppler ultrasonography (DUS) examination. Because many men with PD have avoided coitus for months to years, they are often uncertain of their potency. Severe curvature may preclude intromission, and patients may not appreciate the quality of their erections or the presence of venoocclusive dysfunction. In these men, a home trial of PDE-5 inhibitors with sexual stimulation and subsequent follow-up history regarding the quality of the erections is helpful in choosing the best surgical procedure. In a report by Mulhall and colleagues, 81% of men who complained of some degree of ED on initial assessment responded to medical therapy with PDE-5 inhibitors or home ICI and were able to avoid implantation of an IPP. When erection quality remains unclear, or ED of some degree is likely, ICI with DUS is helpful in identifying abnormalities in penile hemodynamics, plaque location and size, presence of calcification, and degree of curvature. Others have suggested that subclinical penile abnormalities and aberrant communicating vessels that could contribute to postoperative ED if damaged during surgery are able to be noted on ICI/DUS as well. While dynamic infusion cavernosometry and cavernosography (DICC) has evolved as the gold standard for evaluating penile blood flow, peak-systolic and end-diastolic velocities (PSV and EDV) as well as their resultant resistive index (RI) obtained by DUS have been validated as adjuncts to this time-consuming and cumbersome undertaking. A recent article has preliminarily suggested that a RI of less than 0.8 on DUS is predictive of postoperative ED in patients undergoing PD surgery, and thus should be used as the cutoff for recommending IPP rather than corporoplasty or grafting. In any case, severe reduction in blood flow or severe venoocclusive ED should suggest that that prosthesis implantation would be the most successful choice. Digital photography at the time of ICI/DUS can be valuable in determining the severity of PD, planning surgical intervention, and counseling patient and partners as to realistic surgical outcomes.
The importance of proper preoperative assessment of erectile function cannot be overstated. In a recent series, Levine and colleagues reported that among 37 men undergoing grafting procedures for correction of PD, the only preoperative determinant of postoperative development of frank ED was patient-reported preoperative diminished rigidity. Furthermore, Mulhall and colleagues showed that when grafting was used in patients with preoperative diminished rigidity that was responsive to medical therapy (PDE-5 or ICI with Trimix), overall sexual satisfaction decreased significantly postoperatively, whereas this was not the case with patients who underwent corporoplasty. Thus, baseline erectile function is important not only in the decision to proceed with IPP placement but also in deciding between corporoplasty and grafting.
Tunica-shortening or plication procedures are the least invasive surgically and seem to offer the best results with regard to postoperative ED, but are not advisable for all candidates. Shortening procedures reduce penile length in accordance with the degree of curve being corrected. Therefore, they are only advisable for patients with adequate penile length to undergo additional shortening, and should not be used when the potential loss of length is 20% or more of total penile length. Estimation of the loss of penile length can be made at the time of ICI/DUS by measuring the difference between the concave and convex length of the penis.
Preoperative counseling should include discussions of the patient’s and partner’s expectations, alternative treatments, and the risks, complications, and potential outcomes of surgery. As discussed by Nelson and colleagues, the significant psychosocial impact of PD leads many men to a depressed state with poor self-image, and thus many will have overly optimistic expectations as to what is attainable with surgical reconstruction. Because of this, the preoperative discussion needs to be frank and include details as to realistic expectations and surgical limitations. Complications, though generally uncommon, should be discussed, and include penile shortening, glans hypoesthesia, ED, recurrence of curvature, hematoma, and graft contraction. Most patients will require the use of PDE-5 inhibitors postoperatively for penile rehabilitation, and this should also be discussed preoperatively.
Evaluation of patients for surgery
Key factors in evaluating patients for proper placement in the surgical treatment algorithm are degree and complexity of curve, baseline penile length and percent of estimated loss of length with correction, and baseline erectile function. All of these factors are easily evaluated, mostly through physical examination, with the exception of baseline erectile function.
Determining a patient’s baseline erectile status is of prime importance in selecting the surgical treatment that will lead to a satisfactory outcome. Potency may be evaluated by sexual history, a phosphodiesterase-5 (PDE-5) inhibitor take-home test, or intercavernosal injection (ICI) ± Doppler ultrasonography (DUS) examination. Because many men with PD have avoided coitus for months to years, they are often uncertain of their potency. Severe curvature may preclude intromission, and patients may not appreciate the quality of their erections or the presence of venoocclusive dysfunction. In these men, a home trial of PDE-5 inhibitors with sexual stimulation and subsequent follow-up history regarding the quality of the erections is helpful in choosing the best surgical procedure. In a report by Mulhall and colleagues, 81% of men who complained of some degree of ED on initial assessment responded to medical therapy with PDE-5 inhibitors or home ICI and were able to avoid implantation of an IPP. When erection quality remains unclear, or ED of some degree is likely, ICI with DUS is helpful in identifying abnormalities in penile hemodynamics, plaque location and size, presence of calcification, and degree of curvature. Others have suggested that subclinical penile abnormalities and aberrant communicating vessels that could contribute to postoperative ED if damaged during surgery are able to be noted on ICI/DUS as well. While dynamic infusion cavernosometry and cavernosography (DICC) has evolved as the gold standard for evaluating penile blood flow, peak-systolic and end-diastolic velocities (PSV and EDV) as well as their resultant resistive index (RI) obtained by DUS have been validated as adjuncts to this time-consuming and cumbersome undertaking. A recent article has preliminarily suggested that a RI of less than 0.8 on DUS is predictive of postoperative ED in patients undergoing PD surgery, and thus should be used as the cutoff for recommending IPP rather than corporoplasty or grafting. In any case, severe reduction in blood flow or severe venoocclusive ED should suggest that that prosthesis implantation would be the most successful choice. Digital photography at the time of ICI/DUS can be valuable in determining the severity of PD, planning surgical intervention, and counseling patient and partners as to realistic surgical outcomes.
The importance of proper preoperative assessment of erectile function cannot be overstated. In a recent series, Levine and colleagues reported that among 37 men undergoing grafting procedures for correction of PD, the only preoperative determinant of postoperative development of frank ED was patient-reported preoperative diminished rigidity. Furthermore, Mulhall and colleagues showed that when grafting was used in patients with preoperative diminished rigidity that was responsive to medical therapy (PDE-5 or ICI with Trimix), overall sexual satisfaction decreased significantly postoperatively, whereas this was not the case with patients who underwent corporoplasty. Thus, baseline erectile function is important not only in the decision to proceed with IPP placement but also in deciding between corporoplasty and grafting.
Tunica-shortening or plication procedures are the least invasive surgically and seem to offer the best results with regard to postoperative ED, but are not advisable for all candidates. Shortening procedures reduce penile length in accordance with the degree of curve being corrected. Therefore, they are only advisable for patients with adequate penile length to undergo additional shortening, and should not be used when the potential loss of length is 20% or more of total penile length. Estimation of the loss of penile length can be made at the time of ICI/DUS by measuring the difference between the concave and convex length of the penis.
Preoperative counseling should include discussions of the patient’s and partner’s expectations, alternative treatments, and the risks, complications, and potential outcomes of surgery. As discussed by Nelson and colleagues, the significant psychosocial impact of PD leads many men to a depressed state with poor self-image, and thus many will have overly optimistic expectations as to what is attainable with surgical reconstruction. Because of this, the preoperative discussion needs to be frank and include details as to realistic expectations and surgical limitations. Complications, though generally uncommon, should be discussed, and include penile shortening, glans hypoesthesia, ED, recurrence of curvature, hematoma, and graft contraction. Most patients will require the use of PDE-5 inhibitors postoperatively for penile rehabilitation, and this should also be discussed preoperatively.
Tunica-shortening procedures (corporoplasty)
Nesbit and Modified Nesbit
The Nesbit procedure was first described in 1965 for correcting congenital penile curvature caused by corporeal disproportion. Pryor and Fitzpatrick first described the use of the procedure for PD. Plication procedures require that the tunica opposite the Peyronie plaque and penile curvature be excised or plicated, or both, to correct the curvature. After an artificial erection is obtained using injectable saline and the Gittes technique, or with injection of a vasoactive substance into the corpora, an initial circumcising incision is made followed by degloving the penis to the location of the maximal curvature. A ventral penile incision may be used for ventral exposure in very proximal dorsal curvature. Longitudinal penile incisions should be avoided because postoperative scarring can be painful or unsightly, or may even produce further curvature. Buck’s fascia is dissected from the tunica albuginea in patients with dorsal curvature, or it is dissected off the dorsal neurovascular bundles for ventral curvature. After induction of an artificial erection, the point of maximal curve is marked on the convex side of the penis. A 5- to 10-mm transverse ellipse of the tunica albuginea may be excised in the classic Nesbit procedure, or approximately 1 mm for each 10° of curvature.
Rehman and colleagues modified this technique by using a partial-thickness shaving of the tunica to avoid possible bleeding and cavernosal injury. Alternatively, a longitudinal incision can be made at the location of the curvature and closed horizontally in the Heinike-Mikulicz fashion.
Next the tunica is closed in a hemostatic horizontal fashion using either running or interrupted locking, nonabsorbable, braided sutures with buried knots. Nonabsorbable sutures are preferred for maintaining correction during healing, as absorbable sutures are more likely to break, causing recurrence of the curvature. Braided sutures result in fewer knot problems beneath penile skin. A circumcision is recommended in men with redundant foreskin, owing to the increased risk for preputial edema, postoperative phimosis, or preputial necrosis. An artificial erection should again be induced after the tunical closure and, if satisfactory straightening has occurred, Buck’s fascia and the skin can be closed. If extensive dissection has been required it is the authors’ practice to leave a small subcutaneous drain such as the TLS drain (Porex Surgical, Newnan, GA, USA) for 12 to 24 hours to diminish edema. If not adequately straight, subsequent plications or tunical incisions/excisions may be necessary.
A penile block should be administered using long-lasting bupivacaine and a nonpressure dressing and ice pack applied postoperatively. Patients may be discharged home on the same day after this operation. Patients should avoid sexual activity for 6 weeks. The authors’ patients are discharged home on 2 weeks of nightly benzodiazepines for suppression of nocturnal erections, and given amyl nitrate ampoules to be used as needed to suppress additional erections.
Yachia modified the Nesbit procedure by making single or multiple 1- to 1.5-cm incisions longitudinally along the convex side of the tunica, which are subsequently closed horizontally, applying the Heinike-Micwlicz principle. Yachia felt that his modification would reduce injury to the neurovascular bundle and thus reduce glans hypoesthesia, though this known complication is still possible. The authors prefer this approach because tunical deformities and palpable suture lines appear to be fewer. Planning for the tunical incision can be facilitated by placing an Alliss clamp on the tunica to simulate the suture positioning needed to achieve straightening of the penis.
Plication Procedures
Plication of the tunica albuginea is the least invasive technique for correction of PD, and is often performed using only local anesthetic. The predominant techniques used for this include the Lue 16-dot technique, and the tunica albuginea plication (TAP) procedure used by Levine and others. Lue and colleagues describe a 16-dot plication method using multiple plication sutures, with a high patient satisfaction rate. Following induction of an artificial erection, a ventral longitudinal or circumcising incision is performed. Longitudinal incisions are reserved for uncircumcised men desiring to keep their foreskin, and are best performed on the ventral aspect of the penis. Buck’s fascia is incised medial to the neurovascular bundle, and an intravascular space is developed bluntly between the dorsal vein and arteries with subsequent placement of plication sutures in the developed space in a specific 16-point pattern. For men with a dorsal curvature, a ventral longitudinal incision is made down to Buck’s fascia overlying the corpus cavernosum.
After the center-point of the curvature and entry and exit sites for the sutures have been marked, sutures are placed 2 mm lateral to the corpus spongiosum. Two or 3 pairs of 2-0 braided, permanent polyester sutures are placed through the tunica albuginea with 4 entry and exit points per suture. Van der Horst and colleagues found that use of polytetrafluoroethylene sutures resulted in significantly fewer complaints of discomfort by patients than with polypropylene sutures (13% vs 52%) when a similar plication technique was used, whereas Dean and Lue recommend 2-0 braided polyester. The sutures are gradually tied with one surgical knot placed and subsequent clamping. Once all plications are partially tied and clamped, the penis is examined using an artificial erection. If the desired straightening has been achieved the knots are tied and buried, ideally under minimal tension. Buck’s fascia is then reapproximated with absorbable suture and the skin is closed. A penile block is administered with bupivacaine, noncompressive dressing and ice pack are applied, and in most cases patients are discharged on the same day.
Gholami and Lue report that 85% of patients maintained a straight erection while 15% suffered slight or severe curve recurrence in a review of 132 patients at a mean follow-up of 2.6 years. Forty-one percent of the patients in their series reported shortening between 0.5 and 1.5 cm, but this caused functional problems in 7% of patients. Twelve percent reported bothersome knots, 11% erectile pain, 9% penile induration, 6% glans hypoesthesia, and 6% worsened ED.
A modification of the original description of plication by Baskin and Duckett was developed and is used by Levine and others. In this technique, parallel incisions each 1.0 to 1.5 cm in length are made in the tunica and then plicated using 2-0 braided polyester suture in a vertical mattress fashion to bury the knot. If the space between the two incisions is too large dog-ear irregularity of the tunica may occur, and it is recommended that the distance be 0.7 to 1.5 cm between the incisions. If the tunica is significantly thick between the incisions, Levine has had success with shaving down the thickness to reduce the bulk of the plicated tissue.
Licht and Lewis compared the Nesbit, modified Nesbit, and tunical incision and grafting procedures, and found the greatest satisfaction (83%) and lowest ED rates (0%) with the modified Nesbit procedure, but this did not include comparison with plication procedures. More recent studies have echoed these findings, showing satisfaction rates of 67% to 100% with rates of complete straightening of 79% to 100%. Similar rates of satisfaction (78%–83%) and straightening (93%) have been found with the Yachia modification to the Nesbit procedure.
Despite these high satisfaction and successful straightening rates, penile shortening remains an unwelcome outcome of the Nesbit, modified Nesbit, and other plication procedures. In a study involving 359 men, Pryor and Fitzpatrick reported shortening of less than 1 cm in 86.6% of men, between 1 and 2 cm in 8.6%, and greater than 2 cm in 4.7% of men. Similarly, in another large study of 157 men with PD, Savoca and colleagues reported shortening of less than 1.5 cm in 86% of men and between 1.5 and 3 cm in 14% of men. Pryor and Fitzpatrick suggest that the degree of penile shortening rarely precludes sexual activity, noting this outcome in only 1.7% of the men in their study. Analysis of other studies shows that the range for reported sexual dysfunction secondary to shortening is 1.3% to 11.9% for the Nesbit and modified Nesbit procedures. Greenfield and colleagues analyzed the factors affecting the loss of length in their cohort of 102 patients and found preoperative stretched length and degree of curvature to be predictive of the severity of length lost, with an average length lost of 2.4%.
Results vary for plication procedures, with straightening rates ranging from 58% to 100%. Chahal and colleagues reported significantly worse outcomes than Gholami and Lue, with 57% of patients reporting deterioration of their quality of life, 55% severe penile shortening, 48% glans hypoesthesia, and 34% bothersome suture knot nodules.
Known complications with these procedures include curve recurrence (7.7%–10.6%), ED (0%–22.9%), penile indurations or narrowing (0%–16.7%), suture granuloma (0%–1.9%), and glans hypoesthesia (0%–21.4%). Glans hypoesthesia is common postoperatively, though it frequently resolves after several months.
Of note, a new approach to plication has been recently suggested by Dugi and Morey. In their practice they approach all dorsal and lateral plications through a penoscrotal incision, thereby avoiding degloving the penis. Dugi and Morey perform plication using polyester vertical mattress sutures arranged in parallel fashion on the convex side of the penis, and report excellent outcomes, with 93% satisfaction and 2% recurrence in 48 patients. Most notable, however, is their report of no loss of penile length postoperatively, though this measurement was only recorded on the most recent subset of their cohort.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





