CHAPTER 25
Pediatrics
Test Taking Tips
• Remember typical ages at presentation for various congenital disorders that may manifest in similar fashion (eg, duodenal atresia vs malrotation). The age of a neonate can clue you in to the probably diagnosis.
• Many pediatric surgical disorders can be observed for possible resolution. Do not rush to the operative intervention. Examples include umbilical hernias, hernias, and MEN syndromes, where surgery is delayed until a certain age.
Is bilious vomiting a surgical emergency in the newborn and why?
Must rule out malrotation with mid-gut volvulus in a patient with proximal obstruction because the gut can be strangulated (time = bowel).
Differential diagnosis—(memorize this list—the ABSITE will point you toward one of these!) annular pancreas, malrotation, jejunoileal atresia, meconium ileus, meconium plug syndrome, duodenal web/atresia, Hirschsprung, hypoplastic left colon. Always remember 1 anomaly begets additional associated anomalies.
Meconium ileus is associated with what anomaly?
Cystic fibrosis
Duodenal atresia and malrotation are associated with what anomaly?
Down syndrome
What other abnormalities are associated with malrotation?
Diaphragmatic hernia, jejunoileal atresia, abdominal wall defects
Which abdominal wall defects are associated with malrotation?
Both omphalocele and gastroschisis
What is the diagnostic study of first choice to rule in malrotation with midgut volvulus?
Upper gastrointestinal
Surgical procedure for malrotation:
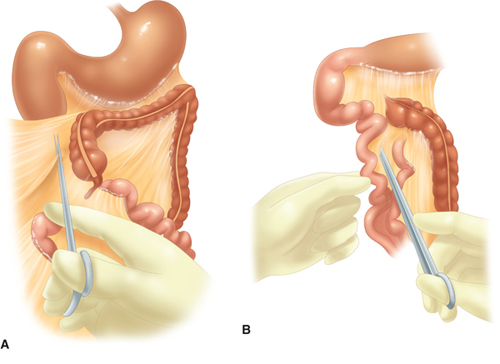
Ladd procedure
Counterclockwise rotation, divide peritoneal bands crossing the duodenum, position SB to right and colon to the left
Look for other abnormalities (see above)
Appendectomy (cecum is now on the left side of the abdomen, perhaps delaying the diagnosis of acute appendicitis.)

FIGURE 25-1. Ladd procedure for malrotation. (A) Lysis of cecal and duodenal bands. (B) Broadening of the mesentery. (C) Appendectomy. (Reproduced from Brunicardi FC, Andersen DK, Billiar TR, et al. Schwartz’s Principles of Surgery. 9th ed. http://www.accessmedicine.com. Copyright © The McGraw-Hill Companies, Inc. All rights reserved.)
FIGURE 25-2. Abdominal radiograph showing the “double bubble” sign in a newborn infant with duodenal atresia. The 2 bubbles are numbered. (Reproduced from Brunicardi FC, Andersen DK, Billiar TR, et al. Schwartz’s Principles of Surgery. 9th ed. http://www.accessmedicine.com. Copyright © The McGraw-Hill Companies, Inc. All rights reserved.)
Why do patients with malrotation have bilous vomiting?
Ladd bands cross the duodenum
Remember that BILIOUS vomiting in newborn is malrotation until proven otherwise.
(most common presentation)
Why is blood flow to the bowel compromised in malrotation?
SMA twisted on its axis—detorsion counterclockwise will relieve this problem. (Malrotation results from failure of normal counterclockwise rotation in utero.)
Duodenal atresia—diagnosis and treatment (Rx):
“Double bubble sign”
Associated anomalies? Prematurity, polyhydramnios (most common), malrotation, annular pancreas, biliary atresia
Resuscitation and then duodenojejunostomy
Rx of duodenal atresia:
Decompression and resuscitation first and then duodenoduodenostomy or duodenojejunostomy
Rx of jeunoileal atresia:
Decompression and resuscitation first then resect atretic portion.
(Run the bowel [common ORALS mistake])!
Patient fails to pass meconium in first 24 hours, bilious vomiting, perforate anus, abdominal distention. “Babygram” shows terminal ileum is dilated; bowel contents have ground glass/soap bubble appearance without air/fluid levels. What is the diagnosis and Rx?
Simple meconium ileus
Rx is gastrograffin enema, pancreatic enzymes, and mucomyst
Get a chloride sweat test post-op
If patient is toxic → (Complicated meconium ileus) resuscitate and go to the OR (Don’t mess with mucomyst when a patient is toxic!).

FIGURE 25-3. Techniques of intestinal anastomosis for infants with small-bowel obstruction. (A) End-to-back anastomosis. The distal limb has been incised to create a “fish mouth” to enlarge the lumen. (B) Bishop-Koop anastomosis. The proximal distended limb is joined to the side of the distal small bowel, which is vented by “chimney” to the abdominal wall. (C) Tapering anastomosis. A portion of the antimesenteric wall of the proximal bowel is excised, with longitudinal closure to minimize disparity in the limbs. (D) A Mikulicz double-barreled enterostomy is constructed by suturing the 2 limbs together and then exteriorizing the double stoma. The common wall can be crushed with a special clamp to create 1 large stoma. The stoma can be closed in an extraperitoneal manner. (Reproduced from Brunicardi FC, Andersen DK, Billiar TR, et al. Schwartz’s Principles of Surgery. 9th ed. http://www.accessmedicine.com. Copyright © The McGraw-Hill Companies, Inc. All rights reserved.)
What is the difference between “meconium plug” and “meconium ileus?”
Meconium ileus is a misnomer. It is actually a distal obstruction. Meconium plug may be secondary to maternal condition, Hirschsprung or cystic fibrosis. It is also a distal obstruction. With passage of the meconium, the obstruction may be relieved.
Called to see a newborn, 27 weeks’ gestation, acidotic, fever, free air on AXR, first stool was bloody. Diagnosis and Rx:
Necrotizing enterocolitis (NEC)!
Make the ABSITE push you to the OR on this one.
Free air
Relative indications for OR. Clinical deterioration, worsening acidosis, persistent fixed loop on abdominal x-ray (AXR), thrombocytosis, portal venous air, abdominal wall erythema/cellulitis, positive paracentesis cultures. Portal venous gas and pneumatosis alone are not absolute indications for OR.
Nonoperative management is NPO, IVF, nasogastric tube (NGT), broad-spectrum IV antibiotics, correct coagulopathy, correct electrolytes, appropriate resuscitation, serial AXR, and bedside evaluations.
Operative management options:
In the neonatal intensive care unit: On high-frequency jet ventilator and can’t be moved to OR ± extreme prematurity (<1000 g). Peritoneal drain at the bedside.
In the OR: Exploratory laparotomy, resection of dead bowel, bring up ostomies
Before establishing continuity, what study is needed and why?
A distal limb study because of the high incidence of associated strictures.
What is the expected urine output in this patient with NEC?
2 cc/kg
Called to L&D to see a patient with bowels outside the abdomen from defect to right of umbilical cord. Diagnosis and Rx:
Gastroschisis
The first step is always resuscitation.
Cover bowel with moist Kerlix, bowel bag.
“Bad bowel, good baby”—only 10% with associated anomalies. The bowel was exposed to amniotic fluid and looks bad.
Remember they will all have malrotation.
Place bowel in silo and slowly cinch the silo bag over time. The bowel may look congested/purplish in the silo.
Do not try to reduce all viscera into the abdomen at the first operation—will result in respiratory distress and possibly abdominal compartment syndrome
Associated anomalies with omphalocele and gastroschisis:
Gastroschisis—intestinal atresia, malrotation
Omphalocele—skeleton, gastrointestinal (GI) tract, nervous system, genitourinary, GI tract. The most common and worrisome is cardiac, so get a STAT echo before going to the OR.

FIGURE 25-4. Neonate with omphalocele. The liver and bowel herniated through a midline abdominal wall defect and are surrounded by a sac of amnion and chorion from which the umbilical cord emanates. (Reproduced with permission from Woo RK, Albanese CT. Pediatric surgery. In: Norton JA, ed. Surgery. 2nd ed. Copyright © 2008 Springer Science+Business Media, LLC. With permission of Springer Science+Business Media.)

FIGURE 25-5. Neonate with a gastroschisis. The defect is to the right of the umbilical cord, and the bowel has no investing sac. Note edema of the bowel wall and the dilated stomach adjacent to the umbilical cord. (Reproduced with permission from Woo RK, Albanese CT. Pediatric surgery. In: Norton JA, ed. Surgery. 2nd ed. Copyright © 2008 Springer Science+Business Media, LLC. With permission of Springer Science+Business Media.)
Which condition is always associated with a sac, gastroschisis, or omphalocele?
Omphalocele always has a sac (may be ruptured); gastroschisis never has a sac
Where can the umbilical cord be found in gastroschisis compared to omphalocele?
In gastroschisis the umbilical cord if found to the left of the defect; in omphalocele the umbilical cord is attached to the sac
Infant with poor PO intake, life-threatening episodes of apnea (near miss SIDS), chronic cough, arching, recurrent pneumonia, asthma, hoarseness. Most likely diagnosis:
Gastroesophageal reflux disease (GERD)
Preoperative evaluation for GERD:
UGI—exclude other causes of vomiting
Gold standard is pH monitoring.
Endoscopy of esophagus, larynx, and trachea
Management of GERD:
Nonoperative: Thicken formulas, small feeds, acid suppression, modify posture
Operative: Nissen fundoplication
Indication for operative management: Failure of medical management, multiple aspiration, near miss SIDS, esophageal stricture, FTT
TRACHEOESOPHAGEAL FISTULA AND DIAPHRAGMATIC HERNIA
Most common TEF:
Gross type C (Type C—90%, Type A—7%, Type E—3%)
Describe Type C TEF:
Proximal EA (blind pouch)—distal tracheoesophageal fistula (TEF)
What is the 2nd most common TEF?
Type A
Describe Type A TEF:
Pure EA—no TEF
What is the common presentation of Type A TEF?
Newborn spits up feeds, excessive drooling, respiratory symptoms with feeds. NGT won’t pass.
FIGURE 25-6. The 5 varieties of esophageal atresia (EA) and tracheoesophageal fistula (TEF). (A) Isolated EA. (B) EA with TEF between the proximal segment of the esophagus and the trachea. (C) EA with TEF between the distal esophagus and the trachea (D) EA with fistula between both the proximal and distal ends of the esophagus and the trachea. (E) TEF without EA (H-type fistula). (Reproduced from Brunicardi FC, Andersen DK, Billiar TR, et al. Schwartz’s Principles of Surgery. 9th ed. http://www.accessmedicine.com. Copyright © The McGraw-Hill Companies, Inc. All rights reserved.)
AXR finding with Type A TEF:
Gasless abdomen, possibly with a scaphoid abdomen
Describe Type E TEF:
Normal esophagus—distal TEF
Most likely TEF to present in adulthood:
Type E
TEF is part of the VACTERL group of anomalies. Describe VACTERL:
Vertebral (ultrasound), Anorectal (rectal examination, imperforate anus), Cardiac (ECHO), TE Fistula, Renal (check renal ultrasound), Limb anomalies
Surgical management of TEF:
Rigid bronchoscopy, right extrapleural thoracotomy, divide fistula, close trachea, primary repair of esophagus, azygous often divided, ± G-tube. Prior to OR—Sump (NGT) for oral secretions, elevated head of bed, antibiotics, resuscitate, H2 blockers, NPO. Esophagogram to identify length of pouch
Patient with diaphragmatic hernia on the left. Do you expect both lungs to be dysfunctional or just the left?
Both are usually dysfunctional secondary to primary pulmonary hypertension
What percent of diaphragmatic hernia present on the left?
85%
Percent of diaphragmatic hernias associated with other congenital defects?
80%. Again, get an ECHO for associated cardiac defects before going to the OR!
Most common diaphragmatic hernia—located posterior-lateral:
Bochdalek
Rare diaphragmatic hernia—located anteriormedially, posterior to sternum:
Morgagni
When are most diaphragmatic hernias identified?
On prenatal ultrasound (typical presentation—no gastric bubble, bowel in chest, polyhydramnios)
NGT placed in child with Bochdalek hernia. CXR shows:
NGT in chest. Bowels in chest.
Failure of the diaphragm to fuse is called:
Eventration
PEDIATRIC NECK
What branchial cleft cyst is anterior to sternocleidomastoid muscle?
2nd branchial cleft cyst
Where does a 2nd branchial cleft cyst usually pass?
Fistula usually passed through carotid bifurcation and into tonsillar pillar.
Most common branchial cleft cyst?
2nd
Lateral neck, lymphatic malformation:
Cystic hygroma (75% present in posterior neck, 20% in the axilla)
Which branchial cleft cyst presents clinically as a firm mass in suprasternal notch or clavicular region?
3rd
The 1st branchial cleft cyst is often associated with which nerve?
1st branchial cleft cyst found at angle of mandible is often associated with facial nerve.
Midline neck mass draining pus:
Infected thyroglossal duct cyst. Give antibiotics to clear infection then Sistrunk procedure (excise tract and central portion of hyoid bone)
Patient presents with cervical lymphadenopathy suspected to be from URI who subsequently fails to respond to 10 days of antibiotics. Possible etiology:
Lymphoma (if it persists). Always check the scalp for a hidden infection.
Patient presents with head persistently rotated. Head noted to be rotated in the opposite direction of the affected muscle. Diagnosis and Rx:
Torticollis. ROM exercises (physical therapy)
TRAUMA
What size airway?
Uncuffed endotracheal tube if less than 8 to 10 years of age. Size is (4 + pt age)/4. Or can use the size of their pinkie as a clue! Remember, no cricothyroidotomy less than 12 years of age
IVF bolus? How much?
20 mL/kg. Blood if no response to 2 IVF boluses
Number 1 cause of death for children ages 1 to 20 years of age:
Trauma
Patient’s mother gives a history of a fall that does not match the developmental stage of the child:
Suspect child abuse
Patient presents with history of fall from 15 feet, hypotensive, distended abdomen, open long bone fracture, blood draining from both ears, and an EMS report of decreased breathe sounds on the right. Next step in management:
Airway (ABC’s)
Best indicator of shock:
Capillary refill/tachycardia. Pediatric trauma—children will look OK and then suddenly become very unstable.
PYLORIC STENOSIS
Ultrasound findings:
Pyloric wall thickness
Greater than 3 mm thick
Pyloric channel—greater than 15 mm long. All bilious vomiting does not equal pyloric stenosis. (For example, 20% of duodenal atresia occurs before the ampulla.)

FIGURE 25-7. Fredet-Ramstedt pyloromyotomy. (A) Pylorus delivered into wound and seromuscular layer incised. (B) Seromuscular layer separated down to the submucosal base to permit herniation of mucosa through the pyloric incision. (C) Cross-section demonstrating the hypertrophied pylorus, depth of incision, and spreading of muscle to permit mucosa to be herniated through the incision. (Reproduced from Brunicardi FC, Andersen DK, Billiar TR, et al. Schwartz’s Principles of Surgery. 9th ed. http://www.accessmedicine.com. Copyright © The McGraw-Hill Companies, Inc. All rights reserved.)
Know the mechanism. Remember that they are volume-contracted and have lost H+ in their vomit. The metabolic alkalosis and dehydration are the first things you need to treat. Use 0.9% NaCl boluses. When the baby is urinating, start 0.5% NaCl at 1.5 maintenance. Then replace the K+. Again, we talk about the importance of K+ levels in these patients, but you need a normal HCO3– before going to the OR. This is a semielective procedure.
Electrolyte findings:
Hypokalemic, hypochloremic, metabolic alkalosis
INTUSSUSCEPTION
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree