1. Clear cell renal cell carcinoma (CCRCC)
2. Multilocular clear cell renal cell carcinoma
3. Papillary renal cell carcinoma (PRCC)
4. Chromophobe renal cell carcinoma (ChRCC)
5. Carcinoma of collecting ducts of Bellini
6. Renal medullary carcinoma
7. Xp11 translocation carcinomas
8. Carcinoma associated with neuroblastoma
9. Mucinous tubular and spindle cell carcinoma
10. Renal cell carcinoma unclassified
Recently the International Society of Urological Pathology (ISUP) has reached a consensus to add five new entities as distinct epithelial tumours [2]: tubulocystic renal cell carcinoma (RCC), acquired cystic disease-associated RCC, clear cell (tubulo)papillary RCC, the MiT family translocation RCCs (in particular t(6;11) RCC) and hereditary leiomyomatosis RCC syndrome-associated RCC. In addition three others were proposed for consideration: thyroid-like follicular RCC, succinate dehydrogenase B deficiency-associated RCC and ALK translocation RCC. However, in our present study, we will only consider the 2004 WHO classification as given in the table below.
1.
Clear cell renal cell carcinoma (CCRCC) is the most common histological subtype accounting for 60–70 % and arises from the proximal tubules. In 2–4 % it is a part of inherited cancer syndrome including von Hippel-Lindau (VHL) and Birt-Hogg-Dubé (BHD) syndromes. It is usually single, with only 4 % multiplicity and 3 % bilaterality. Section surface is yellow with variable degree of haemorrhage, necrosis, cystic degeneration and calcification [3] (Fig. 13.1a, b). The clear cytoplasm of the tumour cells is due to loss of lipid and glycogen during tissue processing [2] (Fig. 13.2a, b). Granular eosinophilic cytoplasm indicates high–grade tumour.
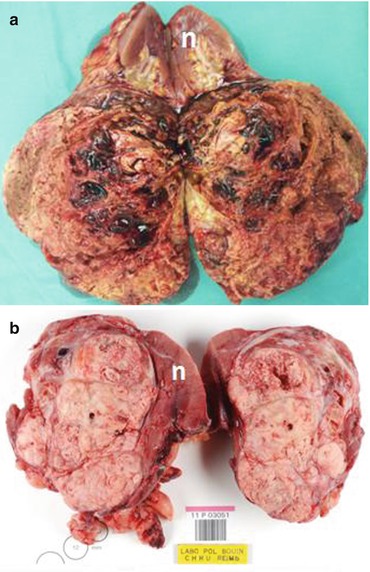
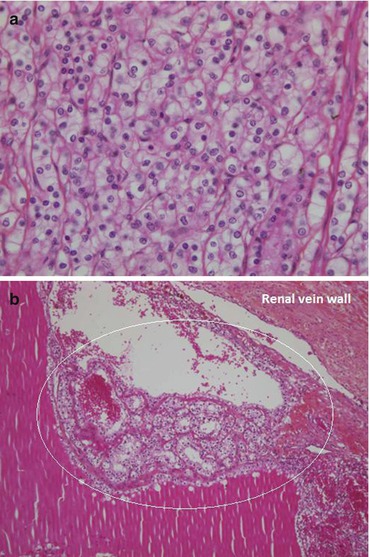
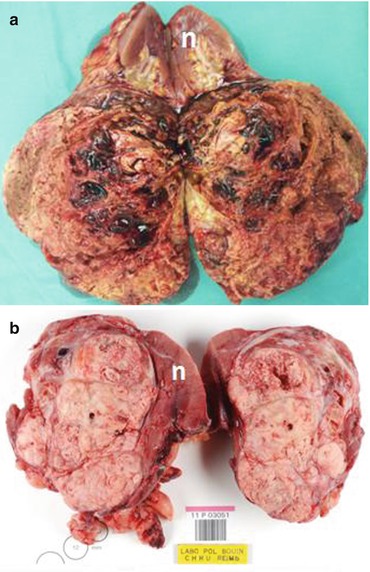
Fig. 13.1
(a) A right radical nephrectomy specimen with a huge CCR (n normal renal parenchyma) (Courtesy of Kurian George, Urology, The Royal Hospital, Muscat, Oman). (b) Section surface of a clear cell RCC with large areas of necrosis (Courtesy of A. Durlach, Pol Bouin Laboratory, University Hospital of Reims, France) (n normal renal parenchyma)
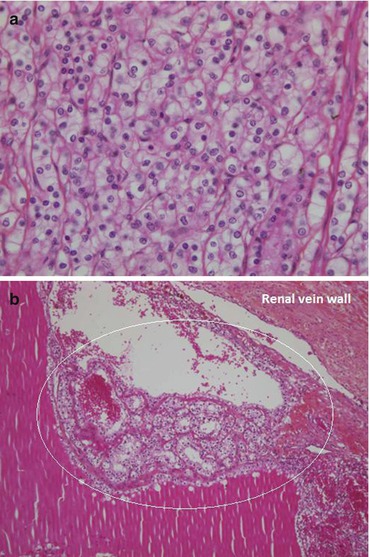
Fig. 13.2
(a, b) Microphotographs of a clear cell carcinoma showing the characteristic clear cytoplasm and a massive tumour thrombus in the renal vein. The circle does not encompass all the embolus (Courtesy of A. Durlach, Pol Bouin Laboratory, University Hospital of Reims, France)
Seventy to ninety percent of CCRCC harbour chromosome 3p alterations. Loss of heterozygosity (LOH) was observed in 78 % of patients with sporadic CCRCC, and almost all the patients showed a likely loss of the whole of the region of 3p examined [3]. Familial VHL cases also exhibited LOH.
VHL protein plays an important role in cellular response to hypoxia through regulation of the hypoxia–inducible factor (HIF), a transcriptional factor. The following sequences are observed [4, 5]:
Normoxic condition → hydroxylation of HIF → recognition and binding by wild-type VHL protein → degradation of HIF within the proteosomes → HIF levels kept at low level.
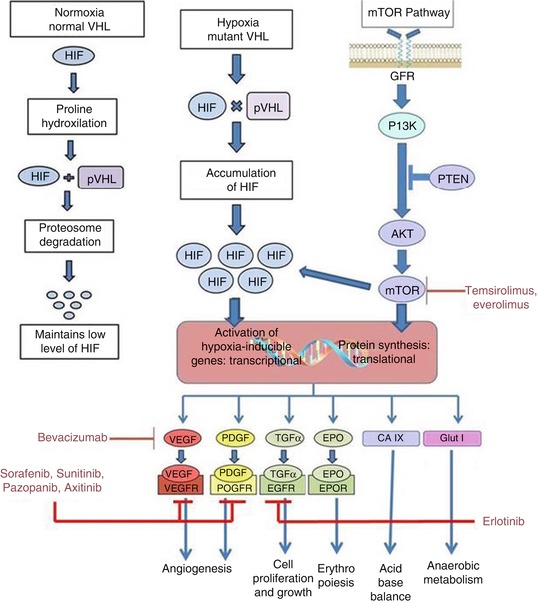
Fig. 13.3
Pathway for VHL and mTOR
These pathways stimulate angiogenesis and compensatory metabolic changes in normal cells when coping with hypoxia [3]. Therefore, inactivation of VHL gene by mutation or hypermethylation results in uncontrolled cellular proliferation leading to tumorigenesis [6, 7].
Another signalling pathway important in RCC is mTOR [8] (mammalian target of rapamycin2). mTOR activation in the presence of phospholipase D enhances the expression of both HIF-1α and HIF-2α in RCC cells [8, 9].
In targeted therapy, critical components of these pathways are targeted as follows:
VEGFR (R = receptor) using neutralizing antibody bevacizumab
VEGFR and PDGFR using small molecule inhibitors of tyrosine kinase such as sorafenib and sunitinib
EGFR (epidermal growth factor receptor) using erlotinib
mTOR using temsirolimus
2.
Papillary Renal Cell Carcinoma (PRCC): Second most common type of RCC accounting for 10–15 %. PRCC usually present at an early stage and has a better prognosis compared to CCRCC of the same stage [10]. The vast majority occurs sporadically; however, there is also a familial variety. They have a well-circumscribed mass enclosed in a pseudocapsule, but some tumours appear necrotic and friable (Fig. 13.4a, b). Bilaterality and multifocality are more frequent than with other RCC varieties [3].
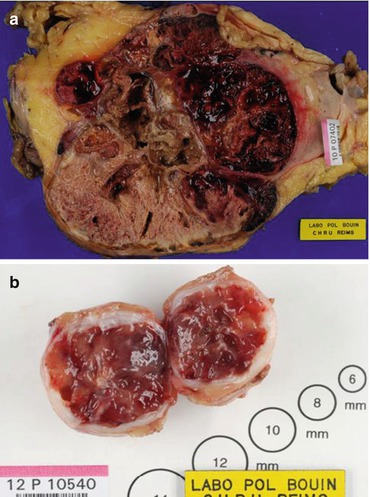
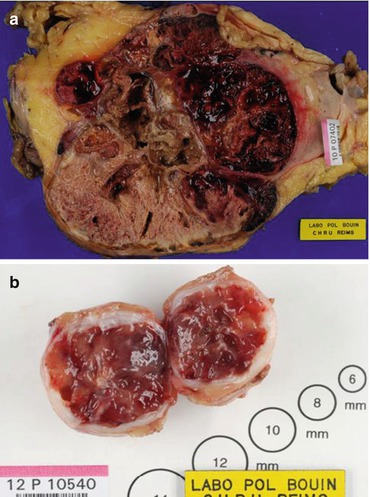
Fig. 13.4
(a, b) Gross specimens of papillary RCC on radical and partial nephrectomy (Courtesy of A. Durlach, Pol Bouin Laboratory, University Hospital of Reims, France)
Two histological types are described [11]:
Type I: Cells with scanty pale cytoplasm. Frequent psammoma bodies and foamy macrophages. Cytokeratin +. They have better prognosis.
Type II: Pseudostratified nuclei, prominent nucleoli, voluminous eosinophilic cytoplasm. They have worse prognosis.
3.
Chromophobe renal cell carcinoma (ChRCC): Accounts for 5 % of RCCs. Believed to arise from intercalated cells of collecting ducts. Prognosis is significantly better than CCRCC. Patients with ChRCC have a low risk of recurrence (<5 %), tumour progression, metastasis and cancer–specific death [12].
4.
Multilocular cystic RCC: 5 % of RCC. Because of their extremely good prognosis after surgery with a 5-year disease-specific survival rate of 100 %, authors have proposed to rename this entity as “multilocular cystic renal cell neoplasm of low malignant potential” [13].
5.
Carcinoma of the collecting ducts of Bellini: Less than 1 % of all renal tumours. They are aggressive tumours with 76 and 19 % of patients found respectively to have pT3 and distant metastases at nephrectomy [14].
6.
Medullary carcinoma: Very rare. Occurs in patients with sickle cell haemoglobinopathy or traits, especially African–Americans and Brazilians. Mean age is 22 years. They are very aggressive with almost all patients presenting with metastasis and dying within 6 months of diagnosis (median survival after nephrectomy: 15 weeks) [15, 16]
7.
The characteristics of the last classified three subtypes of RCC can be summarized as follows [3]: Xp11.2 translocation carcinoma affects children and young adults, accounting for 40 % of RCCs in the latter age group. It is indolent in children but aggressive in adults. The majority of patients with mucinous tubular and spindle cell carcinoma remain disease-free after surgical resection. Post-neuroblastoma renal cell carcinoma occurs in long-term survivors of neuroblastoma with a mean age of 13.5 years (2–35 years), and its pathological features and prognosis are similar to CCRCC.
13.1.1 Fuhrman Nuclear Grading
Fuhrman nuclear grading is a histological predictor of prognosis for CCRCC [17]. First described in 1982, it is based on nuclear size, shape, chromatin and nucleolar prominence and is categorized into 4 grades (Table 13.2).
Grade < div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|
|---|




