Fig. 2.1
Illustration depicting the venous testicular vasculature (a), and the drainage of right and left testes (b). The right testicular vein empties into the inferior vena cava while the left testicular vein drains into the left renal vein
Variant anatomy is seen in about 20 % of cases [32, 33]. Important anomalies include drainage of the right internal spermatic vein into the right renal vein (8–10 %) and multiple terminal spermatic veins (15–20 %). Valves are present in most but not all internal spermatic veins [33].
Theories of Varicocele Origin
Three theories have been postulated to explain the origin of varicocele, which are not mutually exclusive. The first describes the right-angled insertion of the left testicular vein into the left renal vein, with a consequent increase in the hydrostatic pressure that is ultimately transmitted to the pampiniform plexus [26, 34]. The second relies on congenital incompetent (or absent) venous valves, resulting in retrograde flux and dilatation [18, 34]. This theory has been supported by venographic and color Doppler studies. Based upon the level of these incompetent valves being at or below the communicating veins, which include the internal spermatic, cremasteric, vassal and external pudendal veins, two pathophysiologic subtypes have been described, namely shunt and stop types, as shown in Fig. 2.2a and b. When the incompetent valves are located only above the level of the communicating veins, a stop-type varicocele is present, which constitutes 14 % of all varicoceles. The stop-type varicocele is characterized by a brief retrograde flow from the internal spermatic vein towards and into the pampiniform plexus. No orthograde venous blood flow and reflux towards the communicating veins is seen because distal valves are present and are functionally competent. Surgical ligation of the stop-type varicocele shall cure the varicocele by offsetting the reflux-producing incompetent valve against valves from the remaining normal venous drainage system [35]. Conversely, when incompetent venous valves are present below the communicating veins, a shunt-type varicocele is present, which constitutes 86 % of all varicoceles [35, 36]. Shunt-type varicocele is characterized by retrograde blood both from the internal spermatic vein into the pampiniform plexus and orthograde reflux into the communicating veins (vasal and cremasteric veins) [37]. Surgical ligation of the shunt-type varicocele would be expected to be less effective because the incompetent valves are most numerous and widely distributed. Mohseni et al. [38] reported in a prospective controlled study involving 74 children and adolescents with varicocele that the shunt-type was associated with a greater risk of testicular hypotrophy compared to the stop-type varicocele. In addition, the authors noted that a higher recurrence rate occurred when the shunt-type varicocele had been repaired by the retroperitoneal approach compared to the inguinal approach.
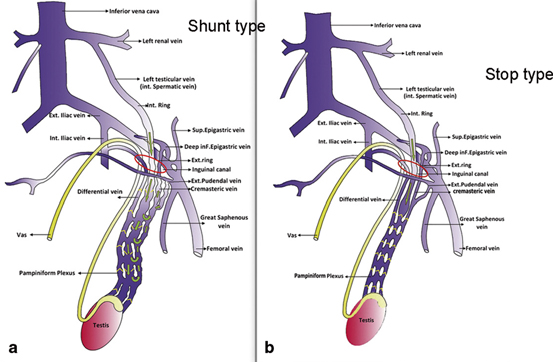
Fig. 2.2
a Schematic anatomy of the shunt-type varicocele shows incompetent valves and shunting through communicating veins, whereas in b stop-type varicocele, the reflux in the spermatic vein is stopped by a competent valve. (Reprinted with permission from Mohseni et al. [38])
The third theory involves the so-called nutcracker effect, in which compression of the left renal vein between the superior mesenteric artery and abdominal aorta would partially obstruct the blood flow through the left testicular vein and therefore increased the hydrostatic pressure inside the pampiniform plexus [39]. The nutcracker phenomenon builds up a steadily raised renocaval pressure gradient and reflux down the internal spermatic vein, resulting in the development of collateral venous pathways [40–43]. Evidence supporting this theory was provided by hemodynamic studies in adults and children with varicocele. In adults, Mali et al. [40] reported correlation between the renocaval pressure gradient and renospermatic reflux, thus showing that the severity of left renal vein compression in the upright position determines the velocity of retrograde flow in the left spermatic vein and varicocele size.
Selective left renal venography with measurement of the pressure gradient between the left renal vein (LRV) and inferior vena cava (IVC) is the gold standard diagnostic method for assessing the nutcracker effect. Normal length of the left renal vein (LRV) is 6–10 cm and the mean normal LRV diameter is 4–5 mm [7]. The normal pressure gradient between LRV and IVC is 1 mmHg or lower and an elevated gradient > 3 mmHg between the LRV and the IVC can be used as a criterion of diagnosis for left renal vein entrapment [44]. Unlu et al. [45] reported using color Doppler ultrasonography that the aortomesenteric angle of men with varicocele ranged between 6–30°, which was significantly different than healthy adult males (25–50°; p < 0.05). Such an angle further decreases during the Valsalva maneuver in an erect position, resulting in further compression of the LRV.
Doppler ultrasonography can be used as the first diagnostic test in patients with suspected nutcracker phenomenon [43, 46]. The B-mode sonographic measurement of the diameter of the LRV combined with Doppler sonographic measurement of the peak velocity (PV) of the LRV was used to diagnose LRV entrapment syndrome. It has been suggested that the distal-to-proximal diameter ratios and flow velocity ratios exceeding 5.0 represent nutcracker phenomenon cutoff levels [43, 46, 47]. In one study involving 67 men with varicocele, 55 % were demonstrated venographically to have an entrapment phenomenon [48].
The nutcracker phenomenon can be the chief cause of pediatric varicocele. In one report, children with the nutcracker phenomenon had higher grade varicocele and obvious collateral vein formation than did the patients with a lower renocaval pressure gradient [49]. However, the insufficiencies of the internal spermatic vein may be the main cause of renospermatic reflux in patients with a low renocaval pressure gradient [25, 40–42, 50, 51]. In children, the use of Doppler ultrasonography in the diagnosis of nutcracker phenomenon has been limited because the left renal vein sampling area is smaller and the Doppler angle is larger in children than in adults [47, 52].
Lastly, the etiology of varicocele may be a combination of all these mechanisms that are further aggravated by an upright posture. As shown in thin, tall athletic subjects, the incompetence of venous valves and lack of fat support around the left renal vein with narrowing of the aortomesenteric angle may lead to varicocele formation [14].
Is Varicocele a Bilateral Disease?
Historically, 85–90 % of all clinical varicoceles are classified as unilateral left-sided. However, recent data indicate that bilateral palpable varicocele is found in > 50 % of affected men [7, 34]. Such data are in agreement with venographic studies that show bilateral abnormal venous reflux in 84–86 % of men with varicocele [53–55]. This finding might explain the occurrence of bilateral testicular damage in such men, and why there is improvement in semen parameters in only 65 % of men after unilateral varicocele repair [56]. In contrast, isolated right-sided varicocele is found in only 2 % of patients and may be associated with the presence of an obstructive lesion, such as a retroperitoneal or pelvic compressive mass [55].
Pathophysiology
Approximately 80 % of men with varicocele are fertile and have normal fecundity [5, 6]. Although the pathophysiology of varicocele has been extensively studied, no conclusive mechanism fully explains why the remaining 15–20 % are infertile.
Scrotal hyperthermia, hormonal disturbances, testicular hypoperfusion and hypoxia as well as backflow of toxic metabolites are potential mediators of varicocele-mediated infertility [57]. Recently, oxidative stress has been implicated as an important mediator of varicocele-associated infertility [57]. Nonetheless, the reasons why some patients with varicocele are infertile, whereas the majority of patients are not, remain unclear. Such phenomenon may be partially explained as infertility being a combination of both male and female factors, in which a fully functional female reproductive system can compensate male factor deficiencies and therefore result in a successful conception. Different intrinsic susceptibility must exist among men with varicocele, which culminates in the various effects of varicocele on male fertility [34].
Oxidative Stress
Reactive oxygen species (ROS) are byproducts of oxygen metabolism and energy production that act as regulators of vital physiological intracellular processes. In the male reproductive tract, small quantities of ROS have important roles on sperm function—regulating capacitation, acrosome reaction, hyperactivation and the fusion of spermatozoa with the oocyte [58]. By contrast, natural intracellular and extracellular antioxidants (enzymatic and non-enzymatic) scavenge and neutralize the harmful effects stemming from increases in ROS levels. When ROS levels disproportionately increase compared with the neutralizing capacity of antioxidants, or when a reduction in the antioxidant capacity has occurred, oxidative stress usually follows.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



