Fig. 2.1
French position
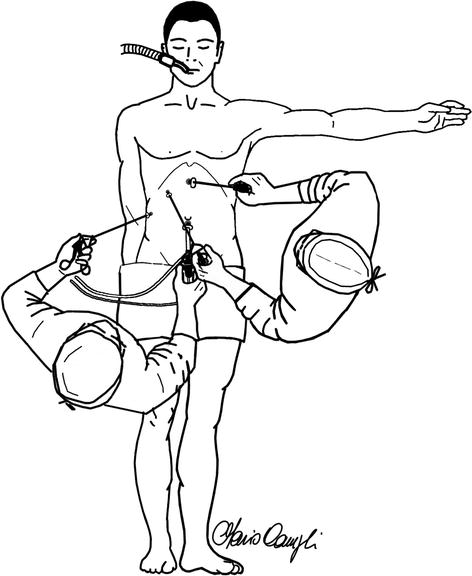
Fig. 2.2
American position
The position of the patient and the surgical team differs between the two techniques: the patient’s legs are divaricated with the surgeon standing between them, in the former, but closed, with the surgeon on the left side of the operating table, in the latter. In both cases, the optical port is at the umbilicus; the operating cannula (for the dissecting instruments) is in the left upper quadrant in the French technique but just below the xiphoid process in the American one. A slight reverse Trendelenburg position and left-sided rotation are enough to allow an easy access to the operating surgeon in the American position, while a steeper reverse Trendelenburg is necessary, in the French position, to bring the operating field closer to the surgeon standing at the pelvis of the patient. The displacement of the liver is trusted to a probe inserted in a cannula positioned just below the costal margin, at the midclavicular line, in the French technique, and the triangle of Calot is exposed by downward and lateral retraction of the gallbladder infundibulum. The American exposure of the surgical field is accomplished, instead, by the assistant who grasps the fundus of the gallbladder, bringing it over the anterior edge of the right lobe of the liver; in this way he rotates upwards the liver itself and exposes the hilum of the gallbladder. In the original American description, the dissection starts at the gallbladder-cystic duct junction, if visible, or high upon the gallbladder otherwise, pulling down the overlying fat until the cystic duct is seen (infundibular technique).
The initial experience demonstrated that the combination of excessive upward traction on the gallbladder and dissection at its infundibulum could be responsible for some common bile duct lesions: the common bile duct can be parallel to the cystic duct, reducing the angle between the two structures, and the choledochus, unduly pulled upwards, can appear in line with the cystic duct and be mistaken for it (Fig. 2.3) [3, 4]. The American technique, then, abandoned the excessive traction on the gallbladder and adopted a lateral retraction of the Hartmann pouch, to keep the cystic duct at an angle with the common bile duct.
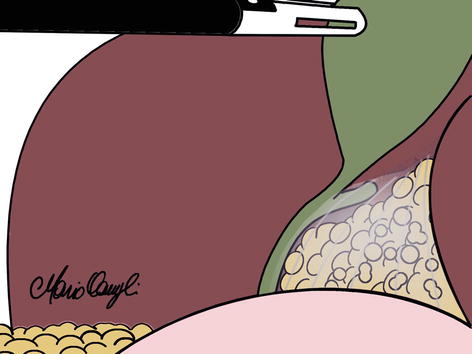
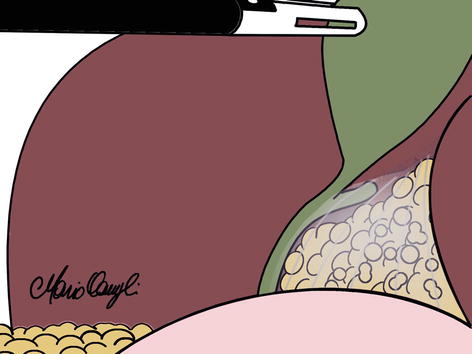
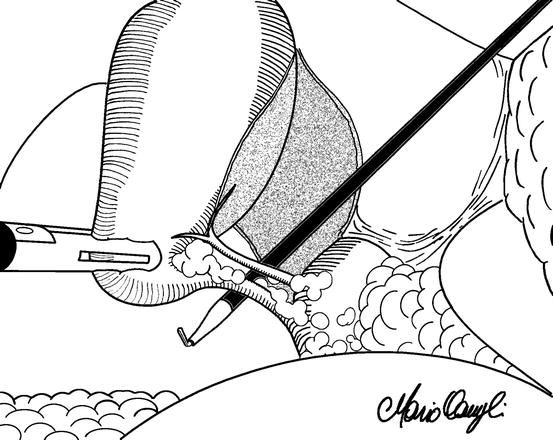
Fig. 2.3
Excessive upward and medial traction can bring the choledochus in line with the cystic duct
On the other hand, the left-sided position of the operating trocar, in the French technique, worried some surgeons. They feared that the passage of the operating instruments from a faraway position towards the surgical fields could provoke some visceral lesion if accidentally introduced without visual control. Therefore, they started adopting the “American” trocar disposition even in an otherwise “French” setting. Beyond description, little has been published about a comparison between the two techniques and how they can affect laparoscopic cholecystectomy performance and outcomes. No evidence-based recommendation can be issued, and the choice is still a matter of personal preference or custom. In particular, no controlled study examined the operative complications of procedures performed with technical details related to these different approaches.
One small randomized trial observed that forced vital capacity and forced expiratory volume in 1 s postoperatively were significantly less after laparoscopic cholecystectomy performed according to the American approach and concluded that the French method leads to less impairment of the respiratory function. The authors put the results into relation with the more cranial position of the trocars in the American technique and to the likely different location of the pain. It has to be observed, however, that the American technique presented in the study includes the extraction of the gallbladder through the epigastric port (while it is most commonly extracted through the umbilical port), and the need to enlarge the incision at this level to allow the removal of the organ could have contributed to the unfavorable result. They also reported one duodenal lesion (out of 23 patients) in the “French” group (LoE2) [5].
There may be several other factors in favor or against one or the other technique. The lithotomy position has been associated with complications rarely occurring in the supine position. These include neurovascular injury to the lower extremities, deep venous thrombosis, compartment syndrome, and osteofascial sclerosis [6]. In addition, proponents of the American position observe that the surgeon between the legs of the patient, stands at a greater distance from the focus of the surgical action and back stretching is often necessary to reach the instruments, despite the greater anti-Trendelenburg angle. Besides, the camera and the arm of the camera driver often interfere with a comfortable position of the surgeon pushed backwards when pan out is necessary. On the other hand, the supporters of the French technique maintain that a better triangulation is achievable, and the surgeon does not need to rotate the trunk and reach over the patient to handle the grasping instrument, with a more comfortable upper limb position. Several studies analyzed the ergonomics of the surgeon’s posture in relation to the position of the monitor, without specifically referring to the differences among the two most common operating room settings. Instead, the effects of the French and American approach have been compared, in regard to surgeons’ learning, performance, and ergonomics, at the Maryland Advanced Simulation, Training, Research and Innovation (MASTRI) Center of the University of Maryland Medical Center [7, 8]. A number of surgeons, at a different level of training, performed four laparoscopic cholecystectomies in a virtual reality surgical simulator. The physical ergonomics were assessed using a tool (“Rapid Upper Limb Assessment, RULA”) developed and validated specifically to investigate the exposure of individuals to risk factors associated with work-related upper limb disorders. Mental workload assessment was achieved through the use of the National Aeronautics and Space Administration-Task Load Index (NASA-TLX). A performance evaluation was also obtained, analyzing the report automatically generated by the simulator at the end of each procedure. According to the scores obtained, the position between the legs of the patient appeared to be the most ergonomically sound from both the physical and cognitive point of view. However, the excellent study has some relevant limitations that can introduce some bias in the conclusions. The performance on the virtual simulator does not necessarily reproduce a real-life situation. In particular, the dimensions of the camera equipment and the distance between the surgeon and the “surgical” field appear to be inferior than in a true operating room situation; the surgeon stands much closer to the optical and operating ports of the simulator than to the respective points on real patients because the simulator does not have legs and pelvis. Therefore, the position of the surgeon’s body, in the French position, does not appear to be as stretched as in real life. Besides, the shorter camera equipment does not appear to interfere with the surgeon’s abdomen, as in real life is often the case. In addition, no data are provided with regard to previous experience of the operators with one or the other examined techniques.
2.3 Technique of Dissection
Since 1990, the beginning of the era of laparoscopic cholecystectomy, Sir Alfred Cuschieri alerted surgeons to be cautious, in order to avoid a rise in surgically induced morbidity [9]. More than 20 years after, the rate of iatrogenic major biliary injury (0.4 %) counts for an almost threefold increase if compared to the traditional open operation (LoE4) [10]. The debate has regained interest since the introduction of new technologies and reduced port surgery for laparoscopic cholecystectomy [11]. An Italian survey confirms an incidence of 0.42 % on major bile duct injuries on 56,591 laparoscopic cholecystectomies, with higher rates in cholecystitis and low-volume practice subgroups (LoE4) [12]. The approach to the gallbladder’s pedicle can be of utmost importance for the prevention of these injuries. Three main techniques have been standardized. The oldest and most common approach is the infundibular one, in which the dissection starts from the infundibulum and deepens into Calot’s triangle. To allow the correct identification of the cystic duct and artery, many maneuvers have been analyzed [4]. Identification of the cystic duct at the junction with the gallbladder is considered the first essential step. Many authors consider mandatory the dissection of the cystic duct until the T-junction of the cystic to the common bile duct could be seen (LoE4) [13]. Once the junction of the cystic duct to the gallbladder and common bile duct was identified, a complete dissection of Calot’s triangle is deemed safe. Other surgeons preferred to stay away from the risk of injuring vascular or biliary anatomical variants, frequently located in the area medial to the cystic duct, and omitted, therefore, a routine search for the common bile duct junction [4, 14]. As a matter of fact, most common bile duct injuries are related to an unclear anatomy, either due to fibrosis and adhesions or to anatomical variations. The latter are quite common in particular within the triangle of Calot [15, 16]. We already mentioned the possibility that a superior and medial traction of the infundibulum could bring the common bile duct in line with the cystic duct; thus the former could be interpreted as the latter and injured (Fig. 2.3). Also, an excessive lateral traction could bring the hepatic artery in the field of dissection (Fig. 2.4). Another “error trap” to avoid is the misinterpretation of the common hepatic duct for the gallbladder wall in severe inflammation [17]. The extension of the cystic duct dissection medially to the confluence with the common hepatic duct might clarify the biliary anatomy like Katkhouda suggests in the “visual cholangiography” technique (LoE5) [18]. Routine intraoperative cholangiography has been advocated by many authors, although its use, especially in emergency, requires a more complex organization of the operating theater and a good expertise of the surgical team. Alas, it does not seem to prevent biliary injuries, even if it helps their immediate identification (LoE4) [19].
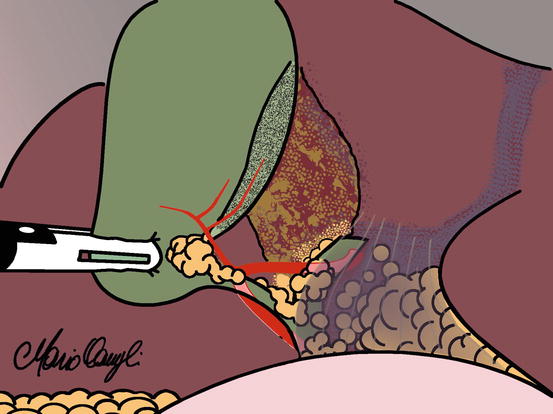
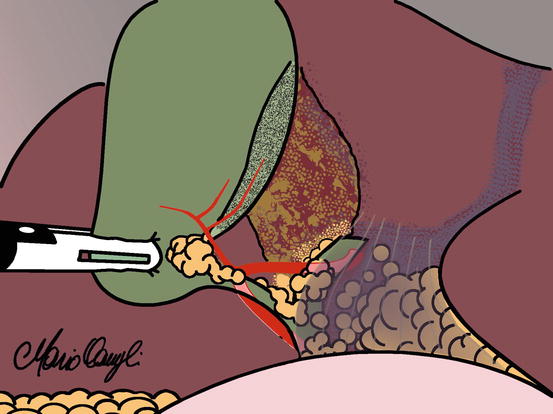
Fig. 2.4
Excessive lateral traction can pull the hepatic artery into the field of dissection
Strasberg, in the early 1990s, introduced the “critical view of safety” (CVS) which involves the dissection of the entire infundibulum from all the fatty tissue, both in its dorsal and ventral aspects (LoE2) (Fig. 2.5) [20]. These principles have been unattended until recent years, in which a standardization of the technique, together with some consistent data confirming Strasberg’s hypothesis, has been published (LoE4) [21, 22]. The results seem promising, as in a series of 3,042 patients, where the observed BDI rate lowers of an order of magnitude, thus overwhelming the results of routine cholangiography (LoE4) [23]. The approach is considered viable even for NOTES gallbladder surgery (LoE5) [24]. The validity of the technique has been tested even in acute cholecystitis (performed by entering the inner subserosal layer for dissection) (LoE4) [25]. Even if there is no comparative evidence to prove a reduction in the bile duct injuries with the use of this technique, it is now widely accepted (even in guidelines) as it does not require additive costs or operative time [26]. An evolution of the concept of critical view of safety is the so-called triangle of safety technique (TST). This approach to the infundibulum is described both in the American and the French trocars’ position [27, 28]. A cephalad hang-up of the fundus is obtained by a grasper, together with the lateralization of the infundibulum. A complete incision of the serosa is performed both in the medial and lateral aspect of the infundibulum and extended upwards almost to the fundus. The medial incision is performed over the vertical fatty line visible on the gallbladder wall; it usually corresponds to the anterior cystic artery which is dissected on the gallbladder surface in order to obtain its medial release. The section of Calot’s artery (which connects the cystic artery to the cystic duct) permits access to the critical safety triangle, set between the gallbladder wall on the right, cystic duct inferiorly, and cystic artery on the left. The entire fatty dissection of this triangle and the mobilization of the infundibulum, both anteriorly and posteriorly, permit the visualization of the liver surface through the triangle, well above Rouviere’s sulcus (Fig. 2.6) in order to obtain the “critical view.” This triangle, which represents the most lateral part of the Calot’s triangle, is generally free of biliary and arterial anomalies, thus permitting a safe and quick dissection, without accidental bleedings which might cause, as a consequence, an inadvertent injury to the biliary ducts [29]. The clipping and the section of the duct, next to the gallbladder, the clipping of the artery and the retrograde dissection of the gallbladder complete the operation. The two cited studies (the former retrospective on 491 patients, the latter a case comparison with the infundibular technique on 174 patients) are not powered to draw conclusions on biliary injuries; alas they acknowledge a reduction of the operative time, a reduction in perioperative morbidity (including intraoperative bleedings), and a null rate of major biliary injuries. These results have been obtained by junior surgeons in both studies, and this reflects increased confidence due to the technique, which probably gives more security to the surgeon, both in inflamed and uninflamed anatomy.