Open Lateral to Medial
Farah Husain
Ira Kodner
Edward Lin
In this section, the open surgical technique with a lateral to medial approach will be outlined.
Location continues to be the major determinant of the type and extent of colon resection, influencing the degree of resection based on the arterial, venous, and lymphatic drainage of the affected colon segment. Furthermore, there is increasing reliance, by medical societies and health care payers, on the adequacy of lymph node resection. Therefore, the number of lymph nodes examined histologically serves as a benchmark of satisfactory oncologic therapy.
Surgical Anatomy
Colon
Topography
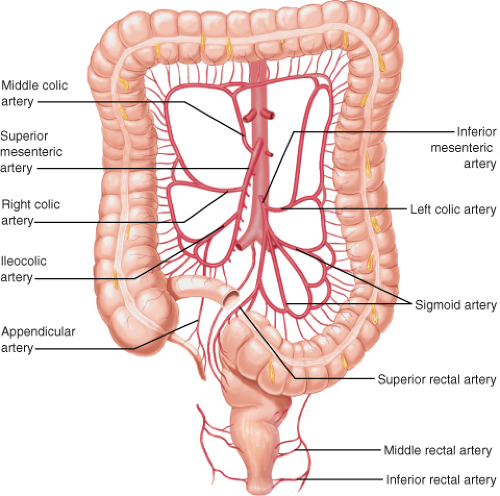
Oncologic colon resection and lymph node harvest are based on the vascular supply of their subsegments. The colon and rectum are derived from the embryologic midgut and hindgut, with the blood supplies following the superior mesenteric artery and inferior mesenteric arteries, respectively. Derivatives of the midgut include the cecum and the right half to two-thirds of the transverse colon. While the derivatives of the hindgut are the left one-third to one-half of the transverse colon, the descending colon, sigmoid colon, rectum, and the superior portion of the anal canal.
Cecum
The cecum is located in the right iliac fossa and is approximately 10 cm long, with the widest transverse diameter of all the colon segments averaging 7.5 cm. It is completely enveloped with visceral peritoneum and is typically mobile. The gonadal vessels and the right ureter typically course posterior to the medial border of the cecum.
The terminal ileum empties from a medial-to-lateral direction into the cecum through a thickened invagination called the ileocecal valve. The valve prevents
retrograde flow from the colon into the small bowel, but in approximately 25–30% of individuals, the ileocecal valve is incompetent. The incompetent valve is most evident during colonoscopies when colonic air readily passes into the small intestines, resulting in marked abdominal distention and patient discomfort. Patients with distal colonic obstructions and functional ileocecal valves typically have colonic dilatation on radiography that mimic a closed-loop obstruction. While the cecum is quite distensible, a diameter greater than 12 cm can result in ischemic necrosis and perforation.
retrograde flow from the colon into the small bowel, but in approximately 25–30% of individuals, the ileocecal valve is incompetent. The incompetent valve is most evident during colonoscopies when colonic air readily passes into the small intestines, resulting in marked abdominal distention and patient discomfort. Patients with distal colonic obstructions and functional ileocecal valves typically have colonic dilatation on radiography that mimic a closed-loop obstruction. While the cecum is quite distensible, a diameter greater than 12 cm can result in ischemic necrosis and perforation.
Ascending Colon
From the cecum, the ascending colon is the 12–20 cm segment that runs upward toward the liver on the right side. With the exception of its posterior surface that is fixed to the retroperitoneum, the ascending colon is covered laterally and anteriorly by visceral peritoneum. The psoas muscle, second portion of the duodenum, the right ureter, and the inferior pole of the right kidney all have important anatomic relationships to the posterior aspect of the ascending colon.
Laterally, the ascending colon is attached to the parietal peritoneum via an embryonic fusion plane between the visceral and parietal peritoneum. This subtle anatomic landmark is relatively avascular and serves as the classic landmark for surgical mobilization of the ascending colon away from its retroperitoneal attachments.
The hepatic flexure of the ascending colon rests under the right liver and turns medially and anteriorly into the transverse colon. The hepatic flexure can often be identified during colonoscopy by a purplish impression on the superior aspect of the colon wall when the scope reaches the right side.
Transverse Colon
The transverse colon is suspended between the hepatic flexure and the splenic flexure on its mesentery and spans 40–50 cm, sharing important anatomic relationships with the stomach, tail of pancreas, spleen, and left kidney. It is completely invested with peritoneum and has a long mesentery known as the transverse mesocolon and may reach into the pelvis. Anatomically, the transverse colon is attached to the greater curvature of the stomach by the gastrocolic ligament or omentum. The greater omentum is attached by a thin relatively avascular membrane to the antimesenteric surface of the transverse colon. Locally advanced tumors of the transverse colon may involve the stomach, pancreas and duodenum posteriorly, as well as the spleen and omentum.
Blood Supply
Arteries
The right colon and up to two-thirds of the proximal transverse colon are derived from the midgut, a region supplied by the superior mesenteric artery. The distal transverse colon and left colon are derived from the hindgut, supplied by the inferior mesenteric artery. All the terminal vessels that vascularize a limited area of bowel wall are supplied by these arteries. Collateralization is excellent along marginal arteries at the mesenteric border, serving as an important source of a segment’s blood supply when a major vessel is occluded. The presence of these marginal arteries also allows the sacrifice of major vessels, facilitating the colon’s mobilization for anastomosis. The lymphatics and innervation of the colon follow the vascular supply.
The superior mesenteric artery (SMA) supplies the entire small bowel with 12–18 jejunal and ileal branches to the left and 3 major colonic branches to the right. The ileocolic vessel is the most constant of these branches and supplies the terminal ileum, appendix, and cecum. The right colic artery is the most variable blood supply of the colon, and may be absent in up to 20% of patients. When present, the right colic artery can originate from the SMA, as a branch of the ileocolic artery or middle colic artery. The right colic artery communicates with the middle colic artery through the marginal arteries.
The middle colic artery is a major blood supply to the colon and is an important surgical landmark when planning a colon resection because it is a demarcation point for the clinical definition of a right or left hemicolectomy (Fig. 2.1). This artery arises proximally as the SMA enters the small bowel mesentery at the inferior border of the pancreas. The middle colic artery then ascends into the transverse mesocolon, and typically divides into the right and left colon blood supplies through the marginal artery. The middle colic may also be absent in some patients and the presence of an accessory middle colic artery may be found in 10% of patients.