Open and Laparoscopic Procedures for SMA Syndrome
Markus W. Büchler
Thilo Welsch
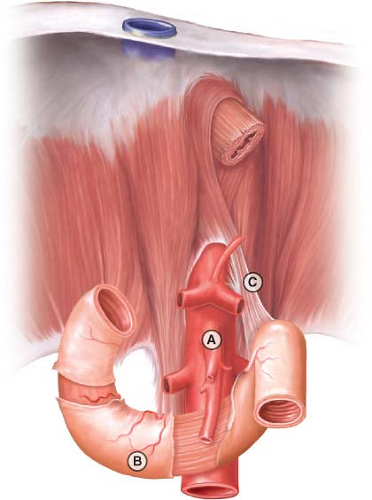
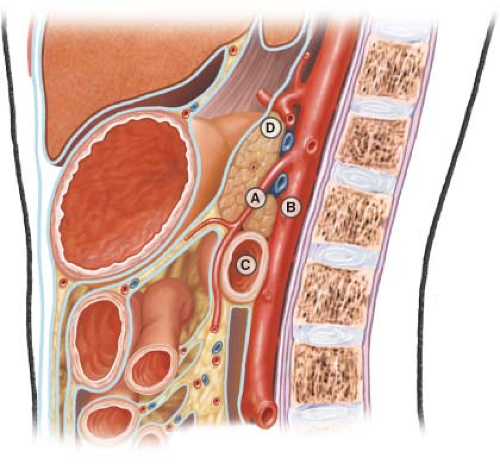
The superior mesenteric artery syndrome (SMA syndrome or Wilkie’s syndrome) is caused by the compression of the third part of the duodenum in the angle between the aorta and the SMA (Figs. 34.1 and 34.2). The entity was first described by the Austrian professor Carl von Rokitansky in his anatomy textbook in 1842. Subsequently, Wilkie published the first comprehensive series of 75 patients in 1927 and his name has become a common eponym for the SMA syndrome. Symptoms arise from the duodenal compression and comprise chronic or acute postprandial epigastric pain, nausea, vomiting, anorexia, and weight loss. Frequently, predisposing medical conditions associated with catabolic states or rapid weight loss result in a decrease of the aortomesenteric angle and subsequent duodenal obstruction. External cast compression, anatomic variants, and surgical alteration of the anatomy following spine or gastrointestinal surgery (e.g., ileoanal pouch anastomosis) can also precipitate the syndrome (Table 34.1).
Once radiologic studies have established SMA syndrome, first-line treatment is usually conservative with jejunal or parenteral nutrition for restoration of the aortomesenteric fat tissue. Nasogastric tube placement for duodenal and gastric decompression and mobilization into the prone or left lateral decubitus position often is effective in the acute setting. If conservative management fails, surgical procedures are indicated and include open or laparoscopic duodenojejunostomy or duodenal mobilization and diversion of the ligament of Treitz (Strong’s procedure). Surgical exploration is further indicated if the SMA syndrome is expected to be caused by vascular pathology or by local tumor growth that require surgical intervention.
Indications for surgical treatment are as follows:
Failure of conservative treatment
Longstanding disease with progressive weight loss and duodenal dilatation with stasis
The need for surgery for the causative pathology
Complicated peptic ulcer disease secondary to biliary stasis and reflux
A detailed history (predisposing medical or surgical conditions, weight loss, epigastric pain, and conservative treatment strategies) and physical examination of the patient is mandatory in the preoperative setting. Patients who present with a history of characteristic symptoms suggesting SMA syndrome should undergo further radiographic studies
to establish the diagnosis. Upper gastrointestinal series, computed tomography (CT) scan or CT angiography, magnetic resonance (MR) angiography, conventional angiography, ultrasonography, and endoscopy have all been used for diagnosis. The following strict radiographic criteria have been established for diagnosis of the SMA syndrome by upper gastrointestinal series with contrast dye: (i) dilatation of the first and second parts of the duodenum, with or without gastric dilatation, (ii) abrupt vertical and oblique compression of the mucosal folds, (iii) antiperistaltic flow of contrast medium proximal to the obstruction, (iv) delay in transit of 4 to 6 hours through the gastroduodenal region, and (v) relief of obstruction in a prone, knee-chest or left lateral decubitus position.
to establish the diagnosis. Upper gastrointestinal series, computed tomography (CT) scan or CT angiography, magnetic resonance (MR) angiography, conventional angiography, ultrasonography, and endoscopy have all been used for diagnosis. The following strict radiographic criteria have been established for diagnosis of the SMA syndrome by upper gastrointestinal series with contrast dye: (i) dilatation of the first and second parts of the duodenum, with or without gastric dilatation, (ii) abrupt vertical and oblique compression of the mucosal folds, (iii) antiperistaltic flow of contrast medium proximal to the obstruction, (iv) delay in transit of 4 to 6 hours through the gastroduodenal region, and (v) relief of obstruction in a prone, knee-chest or left lateral decubitus position.
Table 34.1 Predisposing Conditions for Development of SMAS | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|