Obstetric Magnetic Resonance Imaging
There has been growing interest in the use of magnetic resonance (MR) for maternal-fetal imaging. The great attraction of MR imaging (MRI) in this setting is the ability to produce high-quality images without the use of ionizing radiation. MRI also provides a global view of pertinent anatomy unencumbered by the restrictions of a sonographic window, and rapid MRI sequences allow the production of detailed, motion-free images. Even though there have been no documented adverse fetal effects of MRI, we believe it is usually prudent to avoid imaging in the first trimester of pregnancy (the period of organogenesis).
Technique
Fetal motion limits the choice of pulse sequences. Sequences must be fast enough to be resistant to motion while providing adequate signal-to-noise and tissue contrast. In addition, sequences must be kept within acceptable SAR limits. Currently, the most commonly performed sequence for fetal imaging is HASTE (or ssFSE, ssTSE) (1).
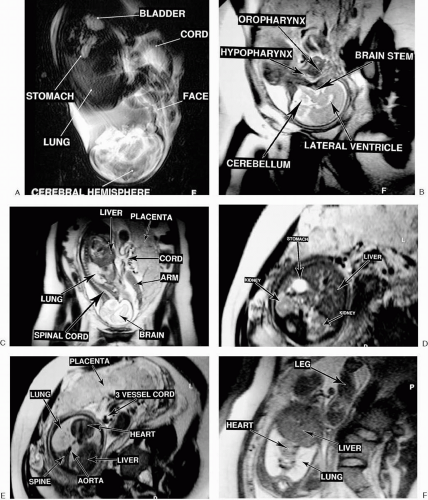
A typical fetal protocol includes a spoiled gradient echo scout sequence to locate the fetus and a series of HASTE images in the axial, sagittal, and coronal planes relative to the fetus. Because of fetal motion, each scan must be planned using the immediate preceding scan as a localizer. To reduce maternal motion, which also contributes to image degradation, images are acquired during maternal breath-holding. The HASTE images provide most of the necessary anatomic information (Fig. 2.70) (2). T1-weighted images may be acquired using a spoiled gradient echo or fast spin echo sequence. Relatively sharp, motion-free images may also be obtained using a steady-state gradient echo sequence (trueFISP, balanced FFE, FIESTA), although the tissue contrast mechanisms are more complex (Fig. 2.71) (3). Steady-state gradient echo sequences produce exceptionally sharp images and have the benefit of relatively low energy deposition in the mother and fetus. Therefore, it is likely that these sequences will eventually become standard for fetal imaging. Gadolinium chelates cross the placental barrier and are not recommended for fetal imaging.
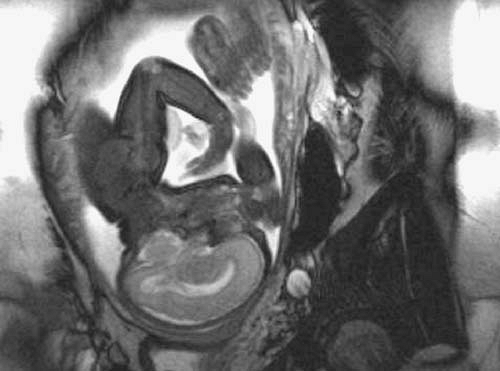 FIG. 2.71. Steady-state gradient echo (trueFISP) sequence for fetal imaging. Anatomy of 32-week fetus is clearly demonstrated. |
Some additional considerations should be taken into account when imaging pregnant women. Prolonged periods in the supine position may be poorly tolerated, particularly during the last trimester. Therefore, sequences should be as short as possible. Placing the patient in an oblique or decubitus position may be necessary to complete the examination. A phased-array body coil improves signal-to-noise ratio but may limit field of view. Maternal abdominal circumference and position may mandate use of the main body coil. Even though no long-term adverse effects of RF exposure from diagnostic MRI on human fetuses have been documented, our collective experience with fetal MRI is still limited. Therefore, one should make an attempt to limit the SAR to the extent possible.
Clinical Applications
Fetal Imaging
Ultrasonography remains the screening procedure of choice for fetal anomalies. However, MRI is useful for evaluating potential abnormalities initially detected with ultrasonography. MRI has several advantages over ultrasonography including decreased operator dependence, superior tissue contrast, independence from the need for a sonographic window, and a larger field of view. Imaging of fetal anomalies may be performed as early as the second trimester.
Suspected brain anomalies are particularly well demonstrated with MRI because of the high image contrast achievable between the brain and CSF, regardless of the fetal head position or degree of calvarial ossification (Fig. 2.72, 2.73). Likewise, detailed normal fetal anatomy is well represented on MR images (4). Early in the second trimester, fetal brain gyration may not be apparent, giving the brain a smooth appearance resembling lissencephaly (Fig. 2.74). At some variable point during the second trimester, fetal brain gyri begin to develop and a layered appearance of the cerebrum can be appreciated. As with ultrasonography, the axial diameter of
the lateral ventricle should not exceed 10 mm beyond 25 weeks of gestation. Fetal spine anomalies, such as meningomyelocele, can also be demonstrated with fetal MRI.
the lateral ventricle should not exceed 10 mm beyond 25 weeks of gestation. Fetal spine anomalies, such as meningomyelocele, can also be demonstrated with fetal MRI.
 FIG. 2.72. Agenesis of corpus callosum. HASTE sequence performed coronal with respect to fetal brain demonstrates dilated, high-riding third ventricle with absence of corpus callosum (arrow). |
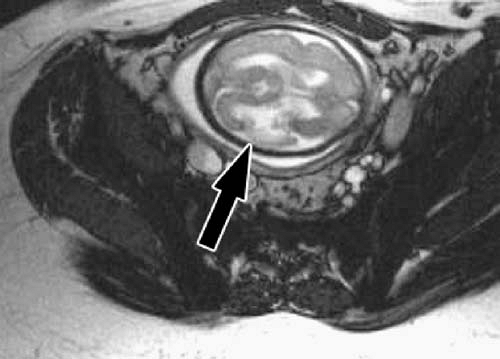 FIG. 2.73. Porencephaly. TrueFISP sequence performed axial with respect to fetal brain demonstrates focal area of porencephaly (arrow). |
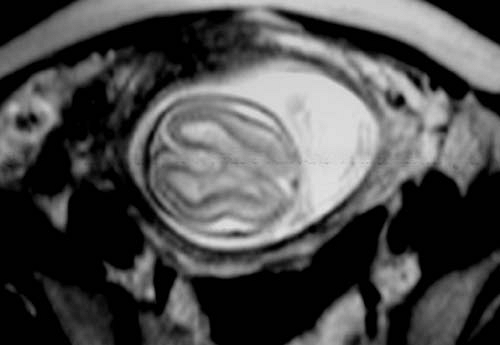 FIG. 2.74. Fetal brain, second trimester. Axial HASTE sequence performed through normal fetal brain early in second trimester demonstrates smooth appearance of cerebral hemispheres. |
Abnormalities elsewhere such as neck masses, diaphragmatic hernias, cystic adenomatoid malformations, pulmonary sequestrations, abdominal wall defects, intestinal and renal abnormalities, and sacrococcygeal teratomas can also be diagnosed or confirmed (5). Fetal contours are clearly outlined by high signal intensity amnionic fluid, which also outlines the oropharynx and proximal gastrointestinal tract. The distal small bowel and colon may appear as high signal intensity on T1-weighted images and low signal intensity on HASTE images (Fig. 2.75) (6). The fetal airways, urinary tract, and gallbladder are also fluid-filled and, therefore, of high signal intensity on the T2-weighted sequences routinely used for fetal imaging. The fetal lung parenchyma is not as bright as amniotic fluid but is still relatively high in signal intensity compared to other organs such as the fetal liver. The umbilical cord and its insertion sites are easily identified. Rarely, fetal cardiac abnormalities may be demonstrated with MRI, although MRI is limited in this capacity due to the small size and rapid motion of the fetal heart.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree