Normal Transnasal Esophagoscopy
The esophagus is a muscular tube that originates in the pharynx and terminates in the stomach. It begins at the level of the 6th cervical vertebrae at the lower end of the cricoid cartilage and averages 20 to 22 cm in length. It traverses the diaphragmatic hiatus at the level of the 10th thoracic vertebrae and ends at the cardia of the stomach at the 11th thoracic vertebrae. The esophageal wall consists of both skeletal and smooth muscle. Striated muscle makes up approximately 5% of the wall of the proximal esophagus. The midesophagus (35%–40%) has a wall of mixed striated and smooth muscle, and the distal 50% to 60% of the esophageal wall is made up of smooth muscle fibers. There is no serosal layer.
The upper esophageal sphincter (UES) is a 2- to 4-cm high-pressure zone which is usually the narrowest portion of the esophagus. It is primarily made up by the cricopharyngeus muscle, which is tonically contracted at rest.
The lower esophageal sphincter (LES) is both anatomic and physiologic. It contains muscle fibers from both the esophagus and diaphragm. The sphincter is thickest on the greater curvature of the stomach and averages 31 mm in length. The fibers are not complete rings but form semicircles and terminate along the anterior and posterior walls of the stomach. The distance to the LES from the nasal ala is approximately 41 cm.
The esophagus is lined by squamous epithelium. At the distal esophagus, the mucosa changes to gastric columnar epithelium. This junction is called the squamocolumnar junction (SCJ), the ora serrata, or the Z-line (Fig. 3.1).
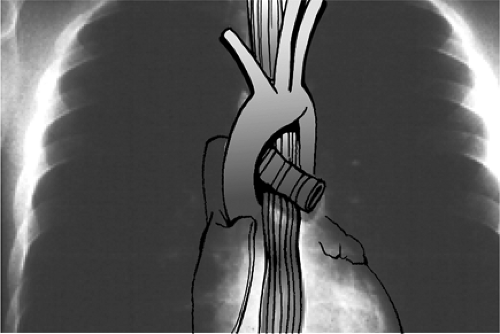 Figure 3.2 The three external compressions of the esophagus, from superior to inferior: the aortic, left main-stem bronchus, and diaphragmatic compressions. |
The anatomy of the esophagus as visualized through the thin transnasal esophagoscope is different from that seen through the transoral endoscope, and is also different from that seen with the rigid esophagoscope. The thin transnasal endoscopes do not distort the normal anatomical relationships, and this allows the normal sphincters, curves, and extrinsic compressions to be easily visualized. The patient is upright in the anatomical position so that left/right and anterior/ posterior can easily be discerned on the monitor.
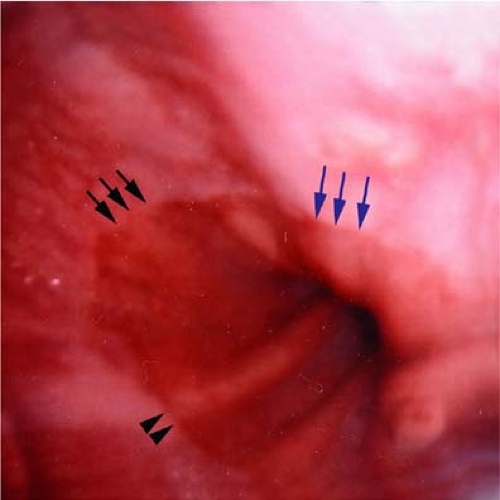
The esophagus starts in the midline and deviates three times before it enters the gastric cardia. The first curve is to the left at the base of the neck. It then curves gently back to the midline at approximately T5. The next curve is to the left again at T7. The final curve is distal, where the esophagus curves anteriorly to pass through the diaphragm. There is also a gentle anterior-posterior curve as the esophagus descends adjacent to the bony spinal column. There are three primary external compressions. From superior to inferior, they are the aortic, left main bronchus, and diaphragmatic compressions (Fig. 3.2). The aortic compression is a pulsatile compression on the left anterior-lateral wall at approximately 24 cm from the nasal ala (Fig. 3.3). The left mainstem bronchus produces an anterior compression at approximately 26 cm from the nasal ala (Fig. 3.4). The diaphragmatic compression occurs at the distal esophagus and produces a lateral and medial constriction (Fig. 3.5). It is best visualized by having the patient perform a sniffing maneuver that opens and closes the diaphragm so that it may be localized.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree