CHAPTER 9 Neurogenic bladder disorders
PATTERNS OF NEUROGENIC DYSFUNCTION
Neurological lesions can be divided into four broad anatomical areas:
Suprapontine
Pattern of dysfunction
Neurogenic detrusor overactivity (NDO) commonly occurs due to reduced cortical inhibitory control of the micturition reflex. As the pontine co-ordination centres are unaffected by this lesion, detrusor and sphincter function co-ordination is preserved; for this reason, patients with suprapontine lesions usually do not develop high pressure neurogenic bladders. However many patients appropriately increase sphincter activity during DO to avoid urgency incontinence, and this increase in EMG activity has been coined pseudodyssynergia. In addition, some patients with cortical lesions lose the ability to voluntarily void and others lose the sensation of bladder fullness and urgency.
Sacral and subsacral
Pattern of dysfunction
A variety of patterns of dysfunction are seen depending on the level of the lesion and the extent of the denervation. A complete sacral or subsacral lesion will lead to an acontractile detrusor, incompetent urethra and loss of bladder sensation. A complete lesion around the conus may demonstrate an acontractile detrusor with a normal or overactive urethra. A complete lumbo-sacral lesion may cause an overactive detrusor with an incompetent urethra. Most lesions are however incomplete and depending on the pathways disrupted can give a varying pattern of dysfunction, e.g. injury to the pudendal nerves may lead to an incompetent urethra whereas an injury to the pelvic nerves may lead to an underactive detrusor with impaired bladder sensation but with a normally functioning urethra. Injury to the afferent axons and pathways may lead to diminished bladder sensation. In addition, incomplete lesions can result in neurogenic detrusor overactivity and high pressure neurogenic bladders.
URODYNAMICS FOR NEUROGENIC BLADDER DISORDERS
In the management of neurogenic lower urinary tract function:
Assessment of lower urinary tract dysfunction is no different from that in neurologically normal patients, consisting of history, examination, voiding diaries, uroflowmetry and pressure flow studies (± EMG). However the interpretation is often more complex and there are specific hazards such as autonomic dysreflexia; therefore the investigations are best performed in specialist centres using video urodynamics. It must be remembered that patients with neurogenic bladder dysfunction also suffer from the same lower urinary tract disorders as the rest of the population, e.g. BOO related to the prostate, and these conditions may further complicate assessment and management. Management should be tailored for each patient depending on the pattern of dysfunction and a plan for follow-up, other relevant investigations (renal function, ultrasound) and repeat urodynamic assessments should be carried out.
NDO AND SPHINCTER OVERACTIVITY (DSD)
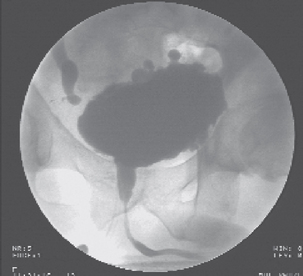
The presence of both NDO and sphincter overactivity is a particularly dangerous urodynamic situation and as a rule of thumb those patients with a competent bladder outflow and a pre-micturition pressure of 40 cm H2O or higher are at particular risk of developing upper urinary tract problems due to the high backpressure, although this is by no means an absolute value and damage to the upper tracts can occur at lower pressures (Figure 9.1). If this pattern of dysfunction is present then the preservation of renal function is of the utmost importance; this requires control of both the NDO and the sphincter overactivity.
Treatment strategies for the NDO include:
Treatment strategies for the overactive sphincter are to ensure adequate drainage; these include:
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree