FIGURE 17.1 Cumulative recurrence rate for stone disease (Uribarri, 1989) (from UpToDate, with permission.)
Medical Conditions Associated with Calcium Stones
■ Hypercalcemia (especially primary hyperparathyroidism and granulomatous disorders such as sarcoidosis)
■ Hypercalciuria
■ Idiopathic (primary)
■ Secondary
• Hyperparathyroidism (also have hypercalcemia)
• Granulomatous disorders (especially sarcoidosis) due to increased conversion of 25-hydroxyvitamin D to 1,25-dihydroxyvitamin D by activated macrophages (may not have hypercalcemia)
• RTA, classic distal type—Failure of H+ excretion results in acidemia, leading to calcium release from bone and hypercalciuria; alkaline urine leads to calcium phosphate stones
Risk of Calcium Stone Formation Relative to Urinary Calcium Excretion | |
|
24-h Calcium (mg/d) | Relative Stone Risk |
<100 | 1.0 |
100–199 | 1.5 |
200–299 | 2 |
>300 | 2.5 |
■ Increased dietary oxalate
■ High-dose vitamin C (metabolized to oxalate)
■ Enteric hyperoxaluria (malabsorption syndromes such as inflammatory bowel disease, leading to decreased calcium-oxalate binding in the gut coupled with bile salt-induced increase in oxalate absorption) (Chadwick et al., 1973; Smith et al., 1972); bariatric surgery (Roux-en-Y gastric bypass) can cause hyperoxaluria, nephrolithiasis and occasionally irreversible renal failure (Nasr et al.,2008))
■ Hyperuricosuria (gout, high animal protein intake; uric acid can serve as nidus for calcium stone formation leading to calcium and mixed calcium/urate stones as well as lead to pure uric acid stones) (Coe et al., 1975)
Inhibitors of Stone Formation
■ Citrate (impairs calcium oxalate lattice formation) (Ettinger et al., 1997; Nicar et al., 1993)
■ Filtered and reabsorbed by proximal tubule
■ Amount reabsorbed dependent on tubular and intracellular pH
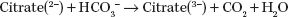
■ Decreased tubular and intracellular pH will increase citrate reabsorption and decrease urinary citrate excretion; treatment with alkali will have opposite effect. Hypokalemia will decrease intracellular pH and urinary citrate excretion
■ Glycoprotein inhibitors
■ Tamm-Horsfall protein (uromodulin)
■ Nephrocalcin
■ Uropontin
Treatment of Calcium Stones
■ Increase fluid intake (Pak et al., 1980)
■ Dietary interventions (decrease protein and sodium intake) (Muldowney et al., 1982)
■ Thiazide diuretics (if at high risk for recurrence, coexistent medical conditions, or recurrent/multiple stones) (Laerum & Larsen, 1984)
■ Potassium citrate (if urinary citrate low) (Ettinger et al., 1997)
■ Allopurinol (if coexistent hyperuricosuria unreponsive to dietary restriction) (Ettinger et al., 1986)
URIC ACID STONES
Risk Factors for Uric Acid Stones
■ Low urine pH and urine volume
■ Gout and/or hyperuricosuria (in some patients) (Yü & Gutman, 1967)
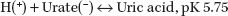
■ Thus, at urine pH 5.75, half of urine uric acid is in relatively insoluble uric acid form
■ Type 2 diabetes increases the risk for uric acid stones (Daudon et al., 2006)
Prevention and Treatment of Uric Acid Stones
■
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


