Chapter 14 Natural Orifice Transluminal Endoscopic Cholecystectomy
Preoperative evaluation, testing, and preparation
Routine preoperative laboratory tests consistent with institutional outpatient surgery guidelines, routine use of a single preoperative dose of intravenous antibiotics, and prophylaxis for deep venous thrombosis are recommended. Patients undergoing TV cholecystectomy should also have a preoperative vaginal bimanual examination by a gynecologist, have a negative Papanicolaou test within the prior 12 months, and undergo bladder catheterization and a povidone-iodine vaginal prep. Other exclusion criteria for both TG and TV cholecystectomy are listed in Table 14-1. Female patients with a contraindication to the TV approach may be considered for the TG approach.
Patient positioning in the operating suite
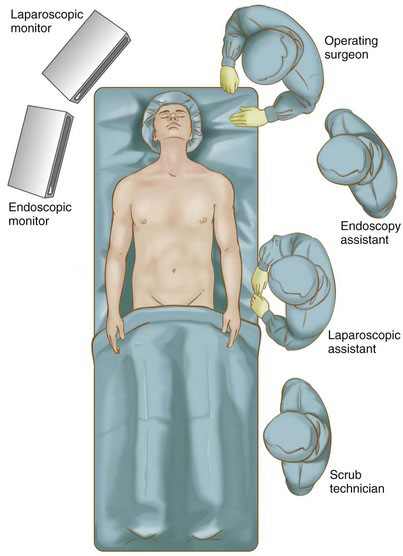
Patients undergoing TG cholecystectomy are placed in a supine position with a flexible anode tube for tracheal intubation. A bite block should be used to help with esophageal intubation with the endoscope or a flexible overtube, or both. The operating surgeon is positioned at the head of the bed cephalad to the left shoulder, with the endoscopy assistant to the left. The laparoscopic assistant is positioned on the patient’s left side with the scrub technician to his or her left. Depending on the type of retraction used, an additional assistant on the patient’s right is helpful. With this setup, all members of the team have good visualization of both the endoscopic and laparoscopic monitors that are positioned on the patient’s right side toward the head (Fig. 14-1).
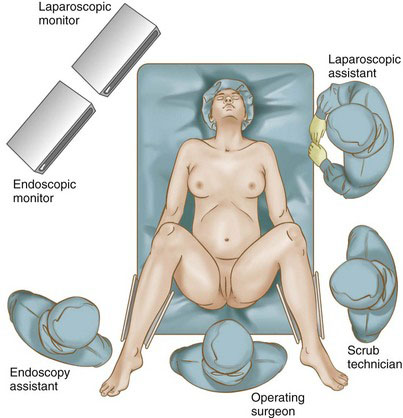
Patients undergoing the TV approach are positioned in a low lithotomy position with the hips not flexed, similar to the position for a laparoscopic sigmoid colectomy. This will minimize any laparoscopic instrument interference with the patient’s left thigh. Careful attention is given to ensuring minimal pressure on the patient’s calves to avoid peroneal nerve injury. The operating surgeon is seated between the patient’s legs, with the endoscopy assistant to the left. The laparoscopic assistant is positioned on the patient’s left side, with the scrub technician to his or her left. The monitors are positioned similarly to the TG approach (Fig. 14-2).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree