Hepatitis C infection is a common cause of cirrhosis and indication for liver transplantation in the United States. The incidence of chronic hepatitis C has been declining, but rates of cirrhosis and hepatocellular carcinoma are projected to increase. The outcome of chronic hepatitis C is variable. It is estimated that 20% to 25% will develop cirrhosis over a 25-year to 30-year period. The rate of disease progression is influenced by many host, viral, and environmental factors. Few can be modified.
Key points
- •
The incidence of chronic hepatitis C is declining in the United States but rates of cirrhosis and hepatocellular carcinoma are projected to increase over the next decade.
- •
Approximately 20% to 25% of patients with chronic hepatitis C progress to cirrhosis over 25 to 30 years.
- •
The outcome of chronic hepatitis C is highly variable and influenced by many host, viral, and environmental factors, many of which cannot be modified.
Introduction
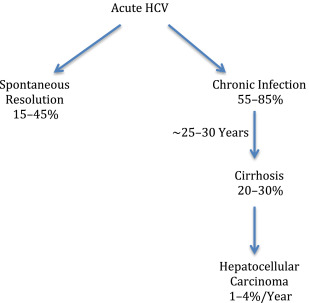
Hepatitis C virus (HCV) infection is an important cause of cirrhosis and hepatocellular carcinoma (HCC) worldwide. It is also a common cause of chronic liver disease in the United States and the leading indication for liver transplantation in the adult US population. The incidence of chronic hepatitis C (CHC) is declining in the United States, but rates of cirrhosis and HCC are expected to increase. Recent data estimate that approximately 1% of the noninstitutionalized US population have chronic HCV infection, corresponding to 2.7 million persons. HCV is primarily transmitted through parental exposure to blood and other bodily fluids. After exposure, an acute hepatitis with jaundice occurs in about 20% of persons, although fulminant hepatitis is rare, occurring in less than 1% of persons. In most cases, the acute infection goes unnoticed. Spontaneous resolution may occur in 15% to 45% of persons and usually occurs in the first 6 months of exposure. The remainder develop a chronic hepatitis that has an unpredictable course. Approximately 20% to 30% of persons with chronic hepatitis progress to cirrhosis over a 25-year to 30-year period. The natural history study of CHC is greatly influenced by host, viral, and environmental factors, most of which are not modifiable ( Table 1 ). In this article, the natural history of CHC is reviewed and the factors that influence its outcome are discussed.
| Host Factors | Viral Factors | Environmental Factors |
|---|---|---|
| Age at infection | Viral load | Alcohol |
| Gender | Genotype | Smoking |
| Race | Coinfection with HBV | Cannabis use |
| Obesity | Coinfection with HIV | Caffeine |
| Steatosis | — | — |
| Insulin resistance | — | — |
| Diabetes | — | — |
| Genetics | — | — |
| ALT levels | — | — |
| Exercise | — | — |
Introduction
Hepatitis C virus (HCV) infection is an important cause of cirrhosis and hepatocellular carcinoma (HCC) worldwide. It is also a common cause of chronic liver disease in the United States and the leading indication for liver transplantation in the adult US population. The incidence of chronic hepatitis C (CHC) is declining in the United States, but rates of cirrhosis and HCC are expected to increase. Recent data estimate that approximately 1% of the noninstitutionalized US population have chronic HCV infection, corresponding to 2.7 million persons. HCV is primarily transmitted through parental exposure to blood and other bodily fluids. After exposure, an acute hepatitis with jaundice occurs in about 20% of persons, although fulminant hepatitis is rare, occurring in less than 1% of persons. In most cases, the acute infection goes unnoticed. Spontaneous resolution may occur in 15% to 45% of persons and usually occurs in the first 6 months of exposure. The remainder develop a chronic hepatitis that has an unpredictable course. Approximately 20% to 30% of persons with chronic hepatitis progress to cirrhosis over a 25-year to 30-year period. The natural history study of CHC is greatly influenced by host, viral, and environmental factors, most of which are not modifiable ( Table 1 ). In this article, the natural history of CHC is reviewed and the factors that influence its outcome are discussed.
| Host Factors | Viral Factors | Environmental Factors |
|---|---|---|
| Age at infection | Viral load | Alcohol |
| Gender | Genotype | Smoking |
| Race | Coinfection with HBV | Cannabis use |
| Obesity | Coinfection with HIV | Caffeine |
| Steatosis | — | — |
| Insulin resistance | — | — |
| Diabetes | — | — |
| Genetics | — | — |
| ALT levels | — | — |
| Exercise | — | — |
Acute hepatitis C
The incidence of acute hepatitis C had been declining in the United States but a marked increase in cases was noted between 2010 and 2013, from 850 in 2010 to 2138 in 2013, representing a 152% increase in cases of acute hepatitis C. This sharp increase has been attributed to an increase in injection drug use among the suburban population in the Eastern and Midwestern states.
The most common symptoms of acute hepatitis C include jaundice, nausea, abdominal pain, and flulike symptoms. In most individuals, HCV RNA is usually detectable within 2 weeks and anti-HCV antibodies within 12 weeks of exposure to HCV. Serum alanine aminotransferase (ALT) levels usually increase within 8 to 10 weeks, with a peak ALT level of 10 to 20 times the upper limit of normal. Serum HCV RNA levels may fluctuate widely during the acute phase and even become negative transiently, only to reappear again. This finding is seen only in the acute phase and may be a clinical clue to the diagnosis of acute HCV infection. Spontaneous resolution occurs in 15% to 25% of individuals and may be up to 45% in persons who present with jaundice, children, and young women. Higher rates of spontaneous clearance were also observed in persons with certain polymorphisms (the rs12979860-C, rs8099917-T, and the ss469415590 TT ) near to the IL28B gene (interferon λ [IFN-λ]). HLA class II alleles may play a role in spontaneous clearance. Less genetic diversity of the viral E1 and E2 envelope genes was observed in individuals with spontaneous recovery compared with those who progressed to chronic infection.
Natural history of chronic hepatitis C
CHC is defined as persistence of HCV RNA in the blood for more than 6 months after the onset of acute infection. About 55% to 85% of patients with acute hepatitis C transition to CHC ( Fig. 1 ). Once the infection becomes chronic, spontaneous resolution is rare. CHC can subsequently lead to progressive fibrosis and cirrhosis, end-stage liver disease, and HCC (see Fig. 1 ).
It is estimated that 20% to 30% patients with CHC progress to cirrhosis. However, this rate is highly variable and dependent on the methodology used to define the natural history of the disease, whether prospective, retrospective, or retrospective-prospective study designs, and the population studied. This factor was highlighted in an analysis of 57 studies undertaken to estimate progression to cirrhosis. Studies were broadly classified as those from tertiary-care liver clinics, posttransfusion cohorts, blood donors, and community-based cohorts. Estimates of progression to cirrhosis after 20 years of CHC varied widely from a high of 24% for posttransfusion cohorts and 22% for tertiary-care liver clinics, to a low of 7% for community-based cohorts and 4% for blood donors. Selection bias, recall bias, and short duration of follow-up probably account for differences in the estimated rate. Community-based cohort studies are likely to provide the best evidence for estimating disease progression at a population level.
Monitoring progression of fibrosis is another way of estimating the outcome of CHC. Because progression of fibrosis is the precursor of cirrhosis, following its progression should reflect the course of the disease. Fibrosis stage was shown to be a good predictor of development of cirrhosis and clinical outcomes, need for liver transplantation, and liver-related death, confirming the importance of fibrosis as a surrogate for outcome of CHC. Cross-sectional biopsy studies estimate a period of 30 years to develop cirrhosis. However, because fibrosis progression is unlikely to be linear, performing repeated liver biopsies in patients should provide a more accurate determination of the rate of progression of fibrosis. Paired liver biopsy studies suggest a time to cirrhosis of 30 to 40 years.
Natural history of cirrhosis
The development of cirrhosis is an important milestone in the natural history of CHC. Once cirrhosis develops, patients are at risk for decompensation, including the development of ascites, spontaneous bacterial peritonitis, variceal hemorrhage, and hepatic encephalopathy. Occurrence of any of these events heralds an increased risk of death or need for liver transplantation. Information on the natural history of hepatitis C after development of cirrhosis has been mostly derived from studies conducted at tertiary referral centers, which may not be representative of all persons with CHC. With this caveat, survival of patients with cirrhosis in the short-term and medium-term is good. Five-year survival ranges from 85% to 91% with a 10-year survival of 60% to 79%. The rate of clinical decompensation is approximately 2% to 5% per year and the development of HCC 1% to 4% per year.
The HALT-C (Hepatitis C Antiviral Long-Term Treatment Against Cirrhosis) trial provided important data on the natural history of patients with advanced fibrosis and cirrhosis. The study treated previous IFN nonresponders with 6 months of peginterferon and ribavirin. Failures to this intervention were then randomized to low-dose peginterferon or observation for the next 3.5 years. After 4 years of follow-up, outcomes occurred at a similar rate between the treated group (34.1%) and the control group (33.8%). The most common clinical outcome was an increase of 2 or more points in the Child-Turcotte-Pugh score (documented on 2 consecutive visits), which occurred in 109 patients (10.4%). Ascites was the most common clinical decompensation event and occurred in 59 patients (5.6%). HCC occurred in 29 patients (2.8%): 13 (2.1%) in the patients without and 16 (3.7%) in those with cirrhosis. Fifty-three patients (5.0%) died, 31 in the treatment group (15 of liver-related causes) and 22 in the control group (12 of liver-related causes). At 3.8 years, the overall death rate was 6.6% in patients who received peginterferon and 4.6% in control patients.
Once decompensation develops, there is an increased risk of death or need for liver transplant. One study followed 200 patients with HCV-related cirrhosis without known HCC after hospitalization for their first hepatic decompensation. During a mean follow-up of approximately 3 years, HCC developed in 33 (16.5%) patients, and death occurred in 85 patients (42.5%). The probability of survival after diagnosis of decompensated cirrhosis was 82% and 51% at 1 and 5 years, respectively. Development of hepatic encephalopathy or ascites as the first hepatic decompensation event was associated with a lower survival rate.
Factors that influence the outcome of chronic hepatitis C
Host Factors
Age at infection
Age plays a major role in the progression of fibrosis. Multiple studies have shown that older age at infection was associated with more rapid progression of fibrosis. In 1 study, 9 host, viral, and environmental factors were correlated with fibrosis progression among 2235 untreated patients who underwent liver biopsy. Fibrosis progression per year was defined as the ratio between fibrosis stage in Metavir units and duration of infection in years. Older age at infection greater than 40 years was independently associated with a faster rate of fibrosis progression.
The reasons for the age-related differences in fibrosis progression are not clear. Alteration in physiologic or immunologic status with increasing age may be important. For example, a decline in liver volume and liver blood flow with aging or decreased immunologic response might contribute to fibrogenesis or fibrinolysis. Alternatively, older individuals may have a greater prevalence of or exposure to factors associated with fibrosis progression. Based on these data, persons older than 50 years should be monitored more closely for disease progression and considered for treatment earlier in the course of their infection.
Gender
Many studies have shown that women have a higher rate of spontaneous resolution of acute HCV infection. Among young women who acquired hepatitis C from receipt of contaminated Rh immune globulin, 45% cleared the infection spontaneously. Similarly, studies of acute hepatitis C among drug users have shown that spontaneous clearance was higher among women compared with men.
Gender also influences the outcome of chronic infection. Men have a higher risk of progression to advanced liver disease, cirrhosis, and HCC when compared with women. Differences in sex hormones have been proposed to explain the gender differences in the progression of the disease. Higher serum testosterone levels were shown to be associated with greater severity of fibrosis. For each 1-ng/mL increase in total serum testosterone, there was a 25% increase in risk of advanced fibrosis. In contrast, estrogen has been proposed to play a protective role in women. In cross-sectional studies, postmenopausal women (with presumed reduced estrogen levels) had higher rates of fibrosis progression compared with premenopausal women, and nulliparous women had higher rates of fibrosis progression compared with multiparous women. In vitro data suggest that estrogen can modify extracellular matrix production and attenuate hepatic stellate cell activation, resulting in less collagen production.
Race
CHC is approximately 3 times more common among non-Hispanic blacks compared with non-Hispanic whites. The prevalence of hepatitis C was similar among Latinos and non-Hispanic whites. African Americans were more likely to be infected with genotype 1, have lower baseline serum ALT levels, less piecemeal necrosis, and less fibrosis, but higher rates of HCC. Latinos were reported to have more severe necroinflammatory activity compared with non-Hispanic whites and a higher prevalence of cirrhosis and HCC compared with African Americans and non-Hispanic whites. A higher prevalence of the metabolic syndrome, insulin resistance (IR), and hepatic steatosis as well as genetic differences among Hispanics are likely important contributing factors.
African Americans and Latinos have lower response rates to IFN-based therapy compared with non-Hispanic whites. A lower prevalence of the favorable IL28b C allele among African Americans and Latinos compared with whites and Asians partially accounts for the lower response rates. Differences in HLA class II alleles influencing host immune response to the virus may also contribute to the racial differences in viral clearance.
Obesity
Obesity, defined as a body mass index (BMI, calculated as weight in kilograms divided by the square of height in meters) greater than 30 kg/m 2 , is an independent risk factor for fibrosis progression and development of cirrhosis. In 1 study, patients undergoing liver biopsy were classified as rapid or nonrapid progressors based on a fibrosis progression rate of greater than 0.2 fibrosis units/y. It was shown that a BMI greater than 25 kg/m 2 was predictive of rapid fibrosis progression. Steatohepatitis associated with obesity and increasing circulating insulin levels are believed to be contributing factors responsible for fibrosis progression in CHC irrespective of the genotype. Obesity is also found to be a risk factor for nonresponse to antiviral therapy independent of steatosis, genotype, and the presence of cirrhosis. Obese individuals have an 80% lower chance of a sustained response to IFN-based therapy compared with normal or overweight patients.
Steatosis
Hepatic steatosis is a common finding among the general population, ranging from 10% to 24%. Using the presence of fat on ultrasonography as a surrogate for steatosis, the prevalence of steatosis was 21% in NHANES-3 (the third National Health and Nutrition Examination Survey) study of the noninstitutionalized US population. The prevalence of steatosis is approximately 2 to 3 times more common in persons with CHC, ranging from 42% to 70%. The cause of steatosis in patients with hepatitis C is multifactorial, resulting from metabolic derangements in the host because of obesity but also because of HCV infection itself. Hepatic steatosis has been suggested to promote the development of fibrosis and hasten progression to cirrhosis, increase the risk for HCC, and lower the response to IFN-based therapy. Nonalcoholic steatohepatitis (NASH) represents a more advanced form of steatosis and has been associated with progressive liver disease and cirrhosis. Therefore, coexistent NASH and CHC may result in more rapid progression of liver disease. Given these adverse consequences of steatosis and NASH, patients with hepatitis C should try to maintain an ideal body weight.
Insulin resistance/diabetes
Diabetes mellitus is a common comorbidity in patients with CHC, ranging from 24% to 62%. The development of IR/diabetes in patients with CHC is complex and seems to be related to presence of the metabolic syndrome as well as a result of the viral infection, both of which may independently lead to the development of cirrhosis. Two meta-analyses have suggested a strong association between CHC and the development of IR. However, some studies have found no association between CHC and prediabetes or diabetes. Rather an association was found with increased ALT and γ glutamyl transpeptidase levels, suggesting that inflammation per se may lead to IR and diabetes. Eradication of HCV has been associated with improvement and even reversal of IR and diabetes.
IR and diabetes are associated with faster progression of fibrosis, increased risk of cirrhosis and its complications (including HCC), and lower response to therapy in patients with CHC. In 1 study of patients with cirrhosis, the presence of diabetes was an independent risk factor for decompensation, liver transplantation, and death. A population-based study from Taiwan reported that new-onset diabetes was an independent predictor of cirrhosis and hepatic decompensation. These findings suggest but do not prove that better control of diabetes or IR could lead to better outcomes among patients with CHC, including those with cirrhosis.
Genetics
Although several host, viral, and environmental factors have been linked with outcome of CHC, they do not completely explain the variable outcome of the disease. A strong host immune response against HCV favors viral clearance. Therefore, variability in genes involved in the immune response may contribute to viral clearance. In a landmark study, a genetic polymorphism near the IL28B gene, encoding IFN-λ3, was shown to be strongly associated with response to treatment with IFN and spontaneous clearance of HCV. The C allele of rs12979860 and G allele of rs8099917 were associated with an almost 2-fold change in treatment-related clearance of HCV compared with the T allele at both loci. This observation was true for individuals of both European and African ancestry. In another study of 1015 patients with chronic infection and 347 who spontaneously cleared the infection, the minor allele (G) of the single nuclear polymorphism at position rs8099917 was associated with a greater than 2-fold progression to chronic HCV infection. The IL28B CC genotype was also shown to be associated with greater hepatic necroinflammation, higher ALT level, and worse clinical outcomes in patients with CHC. Other genetic factors also play a role in outcome of HCV infection but are beyond the scope of this review.
Alanine aminotransferase levels
In population studies, increasing ALT levels were shown to be associated with a progressive increase in death from all causes and in particular liver-related death. Persistently normal ALT levels are found in approximately 20% to 30% of patients with chronic hepatitis. Patients with persistently normal ALT levels are more likely to have mild liver fibrosis on liver biopsy. In a review of 23 studies with more than 1100 patients, 80% of patients with a normal ALT level had mild fibrosis, whereas only 20% had advanced fibrosis. In addition, patients with normal ALT levels progress at a slower rate compared with those with increased ALT levels.
In cross-sectional biopsy studies, serum ALT level was not predictive of severity of fibrosis. However, in paired liver biopsies, increased ALT levels were associated with progression of fibrosis. Serum ALT level was not predictive of development of clinical outcomes; however, the aspartate aminotransferase(AST)/ALT ratio was predictive. Patients with increased serum ALT levels are also found to have increased risk for HCC. In a large Taiwanese study, the cumulative risk for HCC was 1.7% for ALT levels 15 U/L or lower and increased to 4.2% for levels between 15 and 45 U/L and to 13.8% for ALT levels 45 U/L or greater. Therefore, monitoring of ALT levels is useful in managing CHC.
Exercise
Weight loss and exercise are known to cause reduction in steatosis, obesity, diabetes, and IR, leading to improvement in serum ALT levels and fibrosis, despite the persistence of the HCV RNA. The potential benefits of exercise in patients with CHC were shown in a study of 16 obese patients with CHC. Dietary intervention and increased exercise were associated with reduction in BMI, improved insulin sensitivity and serum ALT and AST levels, suggesting that dietary and exercise intervention may improve hepatic and metabolic status in obese IR CHC. The intensity and type of exercise may be important to derive the beneficial effects. High-intensity aerobic exercise training was shown to improve hepatic enzymes and also psychological well-being in patients with CHC. Aerobic exercise has also been shown to improve psychological well-being and quality of life in overweight and obese patients with CHC. Therefore, recommending exercise should be an important component in the management of CHC.
Viral factors
Hepatitis C Virus RNA Level
Unlike human immunodeficiency virus (HIV) infection, there is little evidence to support the notion that HCV viral load affects outcome of CHC. The viral load observed among persons with CHC usually ranges from 10 4 to 10 8 copies/mL, with an average HCV RNA level of approximately 10 6 copies/mL. HCV RNA levels tend to remain relatively stable when serial determinations were made over time and rarely fluctuate above or below 1 log of the baseline. HCV viral load does not differ among viral genotypes. Most studies have shown no correlation between HCV RNA level and histologic outcome. Therefore, there is no role for serially assessing viral load in a patient. Viral load is predictive of response to treatment, with lower viral load being associated with higher response rates.
Hepatitis C Virus Quasispecies/Genotype
The HCV polymerase lacks proofreading capacity, as a result many errors are introduced during replication. Consequently, the virus circulates as a viral swarm or quasispecies. Viral quasispecies were shown to affect spontaneous viral clearance. Lower genetic diversity of the envelope region was associated with a higher rate of spontaneous clearance.
Six major genotypes have been identified based on a sequence divergence of 30% among isolates. HCV genotypes have a geographic distribution, with genotype 1 being the most common worldwide, accounting for 46% of all HCV cases, approximately one-third of which are in East Asia. Genotype 3 is the next most prevalent globally, at 30%. Genotypes 2, 4, and 6 are responsible for a total 23% of all cases, and the remaining cases comprise genotype 5. The association between HCV genotype and disease progression is not clear. A meta-analysis of 16 studies suggested that HCV genotype 3 was associated with accelerated fibrosis progression in single biopsy studies but not paired biopsy studies. It is possible that steatosis associated with genotype 3, an independent predictor of fibrosis progression, might be the cause of the fibrosis progression rather than the HCV genotype 3 itself. The most important clinical usefulness of HCV genotype is as a predictor of response to therapy. The development of HCV regimens with pangenotypic activity may preclude the need for genotyping altogether.
Coinfection with Hepatitis B Virus
HCV shares similar routes of transmission to hepatitis B virus (HBV), so coinfection with these viruses is not uncommon. The prevalence of HBV/HCV coinfection is about 2% to 10%, but there is significant geographic variation. Most studies of HBV-HCV-coinfected patients show that usually only a single virus predominates, although which one was unpredictable. Several studies have shown that coinfected patients are at substantially higher risk for cirrhosis, HCC, and overall mortality compared with HCV-monoinfected patients. In a large US cohort study, a significantly increased risk of cirrhosis (∼89% increase), HCC (∼112% increase), and death (∼62% increase) were seen in HBV/HCV-coinfected patients who were HBV DNA positive compared with monoinfected patients, whereas the absence of HBV replication was associated with a clinical course similar to that of HCV-monoinfected patients. Therefore, patients with HBV and HCV coinfection require close monitoring for the development of cirrhosis and may warrant more intensive HCC screening.
Coinfection with Human Immunodeficiency Virus
HCV and HIV share similar routes of transmission. The overall burden of HIV/HCV coinfection is estimated at 4 to 5 million people worldwide. The prevalence of HIV/HCV varies geographically and by mode of transmission. The highest rates are seen in injection drug users and men who have sex with men. HCV infection is not associated with an increased rate of AIDS-defining events or deaths. However, HIV has several adverse consequences on the outcome of HCV infection. HIV has been shown to increase the rate of chronic HCV infection, to increase HCV RNA levels, and is associated with faster progression of fibrosis and development of cirrhosis. Response rates to IFN-based treatment are also lower among coinfected persons. Before highly active antiretroviral therapy (HAART) therapy, most coinfected individuals died of complications of HIV infection. However, in the post-HAART era, HCV-related liver disease (primarily end-stage liver disease) is a major cause of death among coinfected persons. HIV has been shown to accelerate progression of fibrosis among persons with CHC, including those with persistently normal ALT levels. Approximately one-third of persons with HIV-HCV coinfection progress to cirrhosis over a 20-year period and about 50% progress to cirrhosis over a 30-year period compared with 25% over a 25-year to 30-year period among monoinfected patients.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






