Multidisciplinary Skills for the Internist
Question 1
A 55-year-old woman with a past medical history of hypertension, diabetes mellitus, and proteinuric chronic kidney disease from uncontrolled diabetes is admitted to the hospital with a methicillin-sensitive Staphylococcus aureus bloodstream infection from a tunneled dialysis catheter. Your patient reports a history of penicillin allergy and requests desensitization. All the following statements are true, except
a) It is important to verify the history because the patient may incorrectly assume that a nonallergic side effect, such as a gastrointestinal side effect, is allergic in origin.
b) Fatal reactions to penicillin skin tests have been reported.
c) Skin testing should not be performed in patients with a high risk of an anaphylactic reaction, unless no alternative drug to a β-lactam is available.
d) Patients with a positive skin test to penicillin are at a fourfold increased risk of an allergic reaction to cephalosporins.
e) Desensitization helps reduce the incidence of Stevens-Johnson syndrome, hemolytic anemia, and serum sickness associated with penicillin.
View Answer
Answer and Discussion
The answer is e.
Objective: Identify the benefits of penicillin desensitization.
Desensitization has no effect on the incidence of Stevens-Johnson syndrome, hemolytic anemia, or serum sickness associated with penicillin because these are all non-immunoglobulin E (IgE)-mediated reactions. Fatal reactions to penicillin skin tests have been reported, but they occur in <1% of those tested.
Question 2
The optimal timing for the administration of the pneumococcal vaccination includes which of the following?
a) In the immediate postoperative period after splenectomy
b) Every 10 years in a patient with chronic renal failure who received the vaccination previously
c) In a healthy 55-year-old patient
d) When a person is found to be human immunodeficiency virus (HIV) positive
e) After immunosuppressive therapy, in a patient undergoing organ transplantation
View Answer
Answer and Discussion
The answer is d.
Objective: Identify indications for the pneumococcal vaccination.
The pneumococcal vaccination is recommended in all patients aged 65 years or older. Generally, it should also be given to immunosuppressed patients before their immunosuppression occurs or becomes advanced. Therefore, the vaccination should be given before a planned splenectomy, before the administration of chemotherapy or immunosuppressant therapy, and when HIV infection is first detected. Because of waning immunity, the vaccination should be given every 5 years in a patient with chronic renal failure who received the vaccination previously. Therefore, the correct answer is d.
Question 3
Which of the following statements regarding influenza vaccination is true?
a) It cannot be given at the same time as the pneumococcal vaccination.
b) It is 90% effective.
c) It often causes an influenza-like illness.
d) It is contraindicated in the presence of allergy to eggs.
e) It should not be postponed in the setting of a febrile illness.
View Answer
Answer and Discussion
The answer is d.
Objective: Identify contraindications to influenza vaccination.
A common misconception among patients is that the influenza vaccination causes an influenza infection. The vaccine may cause a local skin reaction, fever, myalgia, and malaise, side effects that the patient may mistake for influenza symptoms. The vaccine does not cause influenza because the vaccine is made from an inactivated virus. The vaccine is contraindicated in those allergic to eggs because the vaccine is made from the inactivated virus grown in eggs. It should be postponed in those with a febrile illness. It is 60% to 80% effective and can be given safely at the same time as the pneumococcal vaccination. Therefore, the correct answer is d.
Question 4
A 50-year-old woman complains of headaches. She has never had headaches before and has no history of neurologic or psychiatric diseases. The headaches began about 6 weeks before and are not severe, but they seem to be getting worse and are beginning to worry her. They wax and wane throughout the day without any particular pattern. They respond well to aspirin but seem to return when the aspirin wears off. They do not wake her from sleep, nor do they cause nausea or vomiting. No neurologic prodrome is present, and she cannot think of anything that exacerbates the pain. It is difficult to localize the headache, and it is not pulsating in character. The pain sometimes improves when her husband massages her neck. No significant past medical, family, or social history is present. She takes no drugs and does not drink alcohol, or smoke. The general physical examination is normal, as is the mental status and cranial nerve examination. The motor examination shows a slight but definite pronation of the left arm on the extension of upper limbs. A careful sensory examination shows some extinction to double simultaneous stimulation on the left. Coordination is normal. Reflexes are symmetric and of average amplitude. Both plantars are flexor. Which of the following is the most appropriate next step?
a) Reassurance
b) Prescribe paroxetine
c) Lumbar puncture
d) Computed tomography (CT) of the head without contrast
e) Magnetic resonance imaging (MRI) of the head with gadolinium
View Answer
Answer and Discussion
The answer is d.
Objective: Identify the indications for imaging in patients with a headache.
This case raises many important issues encountered in the management of a patient complaining of headache. In this particular case, the history itself is worrisome and is enough to warrant further testing. Although the headaches are mild, for this patient, they are different than the usual pattern. This is probably the most important part of the history in a headache patient. Headaches that have changed in quality are more worrisome than severe headaches that are the same as always. The fact that the headaches respond to mild analgesic medication or to massage should not be reassuring to the physician. All sorts of pains respond to analgesic medication, and this in and of itself does not mean that the cause of the headache is benign. Of the greatest importance is the abnormality in the neurologic examination. A slight but definite pronation of the left arm on extension of the upper limbs indicates a mild left hemiparesis. A positive neurologic examination in the presence of headache should always lead to further evaluation. In some centers, it may be possible to do an MRI, but CT scanning is a more widespread and available technology. For this patient, there is really no reason to obtain skull radiographs or any other noninvasive evaluation other than a CT scan. The CT scan may be done without contrast, at which time a lesion may be found. If nothing is found, a decision about injecting contrast can be made later.
Question 5
A 35-year-old man presents to his physician’s office for the first time requesting a “routine physical examination.” He is on no medications, has no significant past medical or family history, and his review of systems is negative. In addition to checking blood pressure (BP), which of the following screening tests would be considered to be most appropriate?
a) Lipid panel, urinalysis, complete blood count
b) Lipid panel, glucose
c) Glucose
d) Lipid panel
e) Lipid panel, electrocardiogram (ECG)
View Answer
Answer and Discussion
The answer is d.
Objective: Identify screening guidelines in a young, healthy patient.
In asymptomatic patients, routine ECGs and screening lab tests, such as urinalysis, complete blood counts, chemistry panels, and liver function tests, are generally not recommended. All major advisory groups recommend BP screening and lipid panel testing by the age of 35 years for all male patients and 45 years for all female patients. High-risk patients are recommended to have screening sooner if they are at increased risk for coronary artery disease. This patient is not at increased risk, and therefore, should have only screening lipids at this time. The U.S. Preventive Services Task Force recommends screening for diabetes in patients with sustained BP greater than 135/85, or at increased risk for impaired glucose tolerance. Assessment for left ventricular hypertrophy, typically with an ECG, is recommended in hypertensive patients only.
Question 6
During a preplacement examination for a bridge reconstruction job, a 32-year-old woman was found to have a blood lead level of 4.0 µg/dL (normal, 0.0 to 11.0 µg/dL) and a zinc protoporphyrin of 104 µg/dL (normal, 0.0 to 70.0 µg/dL). She is asymptomatic and her physical examination is normal. Her medical history is unremarkable, except for four pregnancies. The most likely explanation for these laboratory results is:
a) Unrecognized environmental lead exposure
b) Iron deficiency anemia
c) Erythropoietic protoporphyria
d) Laboratory error
e) Thalassemia minor
View Answer
Answer and Discussion
The answer is b.
Objective: Understand the differential diagnosis of lead exposure.
An elevated zinc protoporphyrin with a normal blood lead level is most often due to iron deficiency anemia, particularly in a woman of reproductive age. Because these studies were obtained during the preplacement evaluation, the patient has not yet encountered lead exposure in the workplace. The physician always should inquire about possible environmental or household exposures, such as the use of glazed ceramic ware, folk remedies, and lead-soldered water pipes. A completely normal lead level excludes recent or ongoing lead exposure from any source.
Erythropoietic protoporphyria is a rare disorder that results in significant symptoms, including photosensitivity. Thalassemia minor and laboratory error are theoretically possible, but highly unlikely explanations for these results.
Question 7
A 42-year-old woman presents with a pruritic erythematous rash around her neck after wearing a new necklace. In the past, she experienced a similar reaction to a cheap pair of earrings. All the following statements are true, except
a) Perfumes and cosmetics can produce the same type of response.
b) Diagnosis can be confirmed with a patch test read in 48 hours.
c) This type of reaction can be caused by topical medications, including antibiotics.
d) Poison ivy produces the same type of response.
e) This is a type II cell-mediated response.
View Answer
Answer and Discussion
The answer is e.
Objective: Understand the mechanisms of hypersensitivity reactions.
Gell and Coombs classification is a classification of the immune mechanisms of tissue injury, comprising four types: type I, immediate hypersensitivity reactions, mediated by the interaction of IgE antibodies and antigens and the release of histamine and other mediators; type II, antibody-mediated hypersensitivity reactions, due to antibody-antigen interactions on cell surfaces; type III, immune complex, local or general inflammatory responses, due to formation of circulating immune complexes and their deposition in tissues; and type IV, cell-mediated hypersensitivity reactions, initiated by sensitized T lymphocytes either by release of lymphokines or by T-cell-mediated cytotoxicity. Contact dermatitis is a type IV cell-mediated response.
Question 8
A 68-year-old woman and her husband are coming in for their annual evaluations. It is mid-November. They have many questions for you regarding prevention. As you begin to counsel them, you remember that which of the following statements is correct?
a) Herpes zoster vaccination is indicated in patients older than 55 years.
b) Prostate-specific antigen and digital rectal examinations are proven screening methods to reduce prostate cancer mortality.
c) Measles vaccine is recommended in individuals born before 1957.
d) Breast self-examination is a proven screening method to reduce breast cancer mortality.
e) The live attenuated influenza vaccine would not be recommended for this couple.
View Answer
Answer and Discussion
The answer is e.
Objective: Identify appropriate screening and immunization guidelines in elderly patients.
Herpes zoster vaccine is recommended for patients aged 60 years and older. Definitive evidence supporting prostate cancer screening is still lacking. Patients born before 1957 are likely to have had the measles virus and need not be vaccinated. Adults born after 1957 who are not previously vaccinated and without demonstrated immunity should receive the vaccine. Advisory groups now list breast self-examination as an optional test because of lack of evidence regarding its effectiveness. Answer e is a true statement—the live attenuated influenza vaccine is only approved for use in patients younger than 50 years.
Question 9
A 45-year-old woman presents to you for a new patient evaluation and wants her “annual physical examination.” Her current medications include an oral contraceptive and ibuprofen as needed. Her mother has a history of hypertension. She is married and works as a legal secretary. Her review of systems is negative. Her previous records report that she had a normal liquid-based Pap smear and a human papilloma virus (HPV) screen 2 years ago. She does not remember any recent lab work and believes that her last immunizations were done when she was a teenager. Which of the following screening tests are most appropriate for this patient?
a) Pap smear, lipid panel
b) Td vaccination, lipid panel
c) Pap smear, Td
d) Td
e) Pap smear, HPV testing, lipid panel, Td
View Answer
Answer and Discussion
The answer is b.
Objective: Identify appropriate screening and immunization guidelines in a healthy patient.
With both a normal Pap smear and negative HPV screen done 2 years ago, this patient does not need another Pap smear for another 3 years. If she just had a normal Pap smear,
but did not have HPV testing, the U.S. Preventative Services Task Force recommends to repeat cytology screening at 3 years. A Pap smear could be done sooner if this patient were considered to be at high risk for cervical cancer. There is no evidence of that in this patient. A tetanus booster immunization should be administered every 10 years after the primary series is completed. Most major advisory groups recommend cholesterol screening in asymptomatic patients with normal risk of coronary artery disease by 35 years of age for men and 45 years of age for women. Therefore, b is the correct answer.
but did not have HPV testing, the U.S. Preventative Services Task Force recommends to repeat cytology screening at 3 years. A Pap smear could be done sooner if this patient were considered to be at high risk for cervical cancer. There is no evidence of that in this patient. A tetanus booster immunization should be administered every 10 years after the primary series is completed. Most major advisory groups recommend cholesterol screening in asymptomatic patients with normal risk of coronary artery disease by 35 years of age for men and 45 years of age for women. Therefore, b is the correct answer.
Question 10
A 68-year-old man is complaining that his handwriting is deteriorating and that his hands shake when he tries to drink from a glass or coffee cup. He has no significant past medical history and no family history of neurologic or psychiatric diseases. He does not drink alcohol, or smoke. His only medication is Sinemet 10/100 four times a day given to him by a physician whom he saw once while on vacation in Florida 2 years before. A physician friend of the patient has been rewriting the prescription since then. His general examination is normal. On motor examination, he is noted to have a rather expressionless face and sits rigidly in his chair with arms flexed, bent slightly forward. Tone is diffusely increased with “cogwheeling.” Power is normal. There is a 2- to 3-second alternating tremor noted in both hands while he is seated. When asked to extend his hands, this tremor becomes finer but more rapid. On finger-nose-finger testing, the tremor intensifies, but no dysmetria is noted. When he attempts to write, the tremor becomes severe, leading to illegible script. The sensory examination is intact. Reflexes are average and symmetric. Both plantars are extensor. His gait is shuffling but with a narrow base. He has difficulty getting started, but, once he is going, he walks quite well although slightly bent forward. Which of the following is the most appropriate treatment plan for this patient’s tremors?
a) Begin metoprolol
b) Begin primidone
c) Increase the Sinemet dose
d) Decrease the Sinemet dose
e) Recommend moderate alcohol consumption
View Answer
Answer and Discussion
The answer is d.
Objective: Identify a physiologic tremor in a patient with underlying Parkinsonism.
This 68-year-old man has two separate problems. The first is a tendency not to move, known as akinesia or bradykinesia. This gives him the expressionless face and accounts for his sitting rigidly in a chair with his arms flexed and bent slightly forward. This akinesia is sometimes referred to as Parkinsonism. In addition to the akinesia, he shows the classic tremor of Parkinsonism, which is characterized as a slow alternating tremor with a frequency of about three cycles per second. This tremor is most prominent in the position of repose and improves when the limb moves into action. When a tremor is superimposed on rigidity, the phenomenon of cogwheeling develops. The tremor of his Parkinson disease is probably not bothering him because it is present only in repose and improves on action. His major complaint concerned the deterioration of handwriting. In fact, he is complaining about a second tremor, some form of postural tremor, which could be either an essential tremor or an exaggerated physiologic tremor. Tremor is defined as an alternating movement around some fulcrum. Tremors may be proximal or distal, rapid or slow, and synchronous or alternating. They may be greatest in the position of repose or on action. Action tremors are subdivided into goal-directed action tremors, which are present only when the patient attempts to make projected precise movements, and postural action tremors, which occur when the affected limb attains an antigravity posture, such as raising the hand. The physiologic tremor is a rapid postural action tremor and is most prominent in the distal extremities and interferes with carrying out fine motor activities, such as writing. It is caused by the peripheral action of catecholamines or their agonists on receptors in the muscle. It is usually not symptomatic, but it may become symptomatic, in which case it is called exaggerated physiologic tremor. Physiologic tremor is exaggerated by situations that increase the sensitivity of peripheral catecholamine receptors or increase the amount of circulating catecholamines. Such circumstances include anxiety, hyperthyroidism, or the use of drugs that functionally raise the circulating catecholamine levels, such as anti-asthmatic medications, lithium carbonate, theophylline, and caffeine. This tremor is treated best by reducing the exacerbating factors or, if necessary, with a small dose of β-blocker. Alcohol is also effective against this tremor, but it is not recommended as a therapy. The second form of postural tremor is known as essential tremor. It is slightly slower than the physiologic tremor, is also present in the extremities most commonly, may occur in families, and may develop only in older people (senile essential tremor). Treatment consists of either β-blocker or use of the antiepileptic drug primidone (Mysoline). Evidence suggests that the incidence of essential tremor is higher in patients with Parkinsonism than in agematched controls; that is, it may be true that the action tremor is part of Parkinson disease. It is also possible that this man has an exaggerated physiologic tremor, possibly caused by the peripheral metabolism of Sinemet to norepinephrine, which then acts on receptors in the muscle. A tremor study done in an experienced neurophysiology laboratory might be helpful in distinguishing these two types of tremor, but a therapeutic trial of reduction in Sinemet may work just as well. In this case, the first choice would be to decrease or discontinue his Sinemet. If there was no effect on the tremor, then treatment with primidone or β-blocker would be appropriate.
Question 11
A 54-year-old woman presents to your office with the chief complaint of vaginal dryness. She became postmenopausal
spontaneously at 52 years of age and has had occasional nondescriptive hot flashes since then. She reports having at least two urinary tract infections in the past year, has noted that sexual intercourse has become more painful over the past year, and has experienced some stress urinary incontinence. Otherwise, she is healthy, has no history of breast or endometrial cancer, and has a normal Pap smear and screening mammogram. She is not interested in systemic hormone therapy (HT) at this time. Your best recommendations are which of the following?
spontaneously at 52 years of age and has had occasional nondescriptive hot flashes since then. She reports having at least two urinary tract infections in the past year, has noted that sexual intercourse has become more painful over the past year, and has experienced some stress urinary incontinence. Otherwise, she is healthy, has no history of breast or endometrial cancer, and has a normal Pap smear and screening mammogram. She is not interested in systemic hormone therapy (HT) at this time. Your best recommendations are which of the following?
a) Vaginal over-the-counter moisturizers and lubricants during intercourse
b) Estradiol vaginal ring
c) Oral contraceptive pills therapy
d) Assessment of bone status
e) Choices a, b, and d
View Answer
Answer and Discussion
The answer is e.
Objective: Identify and manage postmenopausal symptoms.
The use of the estradiol vaginal ring would be an option for local estrogen treatment in a patient with vaginal atrophy and genitourinary symptoms. The estrogen ring provides local estrogen to the vaginal mucosa to help alleviate symptoms of vaginal dryness. The use of nonhormonal over-the-counter vaginal moisturizers and lubricants, including Silk-E and K-Y Jelly, may provide some relief during sexual intercourse. In a woman not on systemic HT, it is important to establish her bone mineral density status because this might affect her decision to initiate HT, or select an alternative therapy with a bisphosphonate (Actonel or Fosamax) or selective estrogen receptor modulator (SERM) such as raloxifene (Evista).
Question 12
A 55-year-old Hispanic woman who became menopausal 3 years ago presents to your office for a routine physical examination. She is currently on conjugated equine estrogens (CEEs) and medroxyprogesterone acetate (Prempro), 0.625 mg/2.5 mg daily, and denies any vasomotor symptoms, sleep disturbances, or change in libido. She does report some “vaginal spotting” twice over the past 3 months. You would recommend which of the following?
a) Bleeding calendar to mark her days of bleeding
b) Hysterectomy
c) Increasing the progestin portion to Prempro, 0.625 mg/5 mg by mouth every day
d) Endometrial biopsy and to consider low-dose Prempro
View Answer
Answer and Discussion
The answer is d.
Objective: Manage postmenopausal vaginal bleeding.
The presence of abnormal vaginal bleeding or spotting in any postmenopausal woman on continuous combined HT should alert the physician to the possibility of endometrial hyperplasia or endometrial cancer. Other causes of spotting include endometrial polyps and uterine fibroids. The next step for therapy would be an endometrial biopsy to further evaluate the endometrial lining for changes. If the endometrial biopsy is benign, consideration should be given to a different HT such as E2/norgestimate (Prefest), E2/norethindrone acetate (Activella), or Femhrt (ethinylestradiol/NA), or low-dose Prempro (0.45/1.5 or 0.3/1.5) (which may offer this patient a better chance of amenorrhea).
Question 13
A 53-year-old white woman with a history of total abdominal hysterectomy with bilateral salpingo-oophorectomy for fibroids, and seizure disorder, presents to your office with the chief complaint of having “hot flashes.” She has been on conjugated equine estrogens (Premarin), 0.625 mg, since her hysterectomy. She is also taking phenytoin and folic acid. She has an isolated elevation of her triglyceride levels to 250 mg/dL. You would recommend which of the following?
a) Adding progestin, 5 mg daily
b) Increasing her oral Premarin dose to 1.25 mg daily
c) Adding isoflavones to her diet and then stopping Premarin
d) Changing her estrogen therapy (ET) to a transdermal patch therapy such as weekly Climara
View Answer
Answer and Discussion
The answer is d.
Objective: Identify drug-drug interactions between estrogen and other medications affecting the hepatic metabolism.
Because of her history of using phenytoin for seizure disorder, this patient probably metabolizes estrogen at a faster rate than normal. By changing her ET to a transdermal patch, consistent estrogen levels can be maintained, which should alleviate her symptoms. Simply increasing her oral CEE dosage does not account for the fluctuations in metabolism and is less favorable than changing to a transdermal patch. Addition of progestin would not help with the hot flashes. Adding isoflavones and other plant-based estrogens in addition to her ET may or may not also help her symptoms. Other causes for her hot flashes should also be excluded, including checking for the thyroid-stimulating hormone and fasting blood sugar level. The patient will also benefit from a transdermal patch therapy instead of the oral ET due to her elevated triglyceride level. Fasting lipid levels should be periodically monitored.
Question 14
A 43-year-old mother of four children presents to the office with complaints of headache, neck pain, some dizziness, and nausea. She has a history of chronic tension headaches and low back pain. She works as a pharmaceutical representative and reports spending a lot of time in her car. She has been seeing a chiropractor on and off for 20 years to treat her chronic symptoms, but despite a visit to the chiropractor
yesterday, her headache remained. She reported nausea right after the visit. While cooking dinner that night she reported dizziness. “I turned my head to the left, and the room started spinning and I felt nauseated. It lasted only a second.” Today she reports similar episodes of spinning that have lasted longer and that were associated with nausea. Physical examination reveals a normal vascular examination without bruits. There is no hearing deficit. Neurologic examination is significant for horizontal nystagmus and left eyelid ptosis. Which of the following is the most likely cause of her vertigo?
yesterday, her headache remained. She reported nausea right after the visit. While cooking dinner that night she reported dizziness. “I turned my head to the left, and the room started spinning and I felt nauseated. It lasted only a second.” Today she reports similar episodes of spinning that have lasted longer and that were associated with nausea. Physical examination reveals a normal vascular examination without bruits. There is no hearing deficit. Neurologic examination is significant for horizontal nystagmus and left eyelid ptosis. Which of the following is the most likely cause of her vertigo?
a) Benign positional vertigo
b) Vestibular neuritis
c) Cerebrovascular stroke
d) Migraine
e) Cholesteatoma
View Answer
Answer and Discussion
The answer is c.
Objective: Identify an ischemic etiology for vertigo.
Vertigo is defined as an illusion of movement and always reflects a disorder of the vestibular system. Vertigo originating from the central nervous system tends to spare hearing, produces less torsional vertigo, and is associated with other brainstem symptoms and signs, such as double vision, dysarthria, and ataxia. The horizontal nystagmus and the eyelid ptosis are concerning for a cerebrovascular stroke and consistent with her recent neck manipulation by her chiropractor. Although uncommon, extreme or abrupt twisting of the neck can damage the inner layer of vertebral arteries.
Question 15
A 48-year-old African American woman with a history of total abdominal hysterectomy and bilateral salpingo-oophorectomy 4 years ago for benign reasons comes to your office complaining of low sexual interest and an inability to reach sexual climax. She is currently on esterified estrogen (Menest), 0.625 mg every day, and denies other symptoms. You check her total serum E2 level, which is 50 pg/mL. She has a normal vaginal and pelvic examination. You recommend which of the following?
a) Sertraline (Zoloft), 25 mg by mouth every day and sex therapy
b) Vaginal lubrication
c) Changing to esterified estrogens, 0.625 mg, plus methyltestosterone, 1.25 mg (Estratest HS) by mouth every day
d) Increasing her dose of Premarin to 1.25 mg by mouth every day
View Answer
Answer and Discussion
The answer is c.
Objective: Identify and treat female androgen deficiency (FAD).
This patient’s symptoms seem to correlate with a FAD, syndrome requiring therapy. Because she is already on adequate estrogen replacement, the only method currently available for androgen therapy is oral Estratest HS (1.25 methyltestosterone and 0.625 mg of esterified estrogen). At present, no agent is the Food and Drug Administration approved for FAD. She should have periodic monitoring of her triglycerides, cholesterol profile, and free and total testosterone level before and after therapy is initiated as there is an increased risk of cardiovascular disease, presumed to at least be partially related to higher levels of total cholesterol and low-density lipoprotein. Also, ˜20% of women can have side effects of hair loss, deepening of voice, hirsutism, and so on, even with testosterone levels within the normal range, although the risk of this increases substantially with supratherapeutic levels.
Question 16
A 56-year-old white woman who has been postmenopausal for 6 years comes to you for a routine examination. She has intermittent symptoms of gastroesophageal reflux disease and has a past medical history of esophagitis. She also had a recent dual-energy X-ray absorptiometry (DXA) scan of her spine and hip that showed a T score of -2.5 standard deviations below young normal. She states her mother was diagnosed with breast cancer, and she is not interested in hormone therapy. She has no personal or family history of deep venous thrombosis (DVT). You recommend which of the following?
a) Medroxyprogesterone acetate (Depo-Provera) injections every 3 months
b) Raloxifene, 60 mg by mouth every day
c) Alendronate, 70 mg by mouth every week
d) Calcium supplementation to a total of 1,500 mg daily with vitamin D, 400 to 800 IU daily
e) Both b and d
View Answer
Answer and Discussion
The answer is e.
Objective: Manage osteoporosis (OP) in a patient with esophagitis.
This patient has OP on DXA, which is of concern and must be treated. Although calcium supplementation at 1.5 g plus vitamin D, 800 IU/day, is necessary but not sufficient to treat OP, she needs additional treatment to prevent further bone loss. The best option for treatment in this patient is a SERM such as raloxifene. Raloxifene will not only prevent further bone loss but also offer her a breast cancer risk reduction, as well as a decrease in the total cholesterol without an increase in the ultrasensitive C-reactive protein. Because of this patient’s past medical history of esophagitis and gastroesophageal reflux disease, Fosamax or Actonel can still be an option for treatment, but the gastrointestinal symptoms would have to be followed closely. Injectable Forteo, a bonebuilding agent, could be considered.
Question 17
A 23-year-old man presents to your office after recently being discharged from the hospital with the diagnosis of new-onset seizures and epilepsy. He is currently taking valproic acid as
prescribed and denies any seizures for the past 2 weeks. He works as an electrician and drives a company van to and from his jobs. He is often climbing ladders and working with “live” wires. Which of the following is the most accurate statement in regard to returning to normal daily activities?
prescribed and denies any seizures for the past 2 weeks. He works as an electrician and drives a company van to and from his jobs. He is often climbing ladders and working with “live” wires. Which of the following is the most accurate statement in regard to returning to normal daily activities?
a) He should not be driving until he has been seizure free for 6 to 12 months.
b) As long as his valproic acid level is therapeutic, he may return to normal activities, including driving.
c) Epileptics, regardless of seizure control, should not climb ladders or work with heavy machinery.
d) He will need approval from the Bureau of Motor Vehicles and a special driver’s license to return to his job.
View Answer
Answer and Discussion
The answer is a.
Objective: Identify appropriate lifestyle recommendations for patients with seizure disorders.
Seizures can be associated with a sudden alteration of consciousness that may interfere with the activities of daily living or put the patient in a dangerous situation. In general, patients should not drive unless the seizures are under control. Each state within the United States has specific rules about what is meant by the phrase “seizure free for a long enough period.” Generally, this period ranges between 6 and 12 months without a seizure while on an appropriate antiepileptic drug regimen. Some states require that the physician report such cases to the Registry of Motor Vehicles; in other states, this is not necessary. Familiarity with local laws on this subject is recommended. Other activities such as swimming, bathing, operating heavy machinery, and climbing great heights are usually not regulated specifically, but should be avoided when unsupervised.
Question 18
A 32-year-old woman with no past medical problems is seen at her primary care physician’s office. She is currently in her 12th week of gestation and was found to have HIV on routine screening. She is seeking further care for this. Which of the following is true?
a) The confirmatory Western blot test may be falsely positive in pregnancy.
b) Untreated, perinatal transmission approaches 60%.
c) Perinatal antiviral treatment will decrease the transmission rate to <7%.
d) Pneumocystis jiroveci pneumonia (PCP) prophylaxis should be started regardless of the CD4 count.
e) Termination of the pregnancy will offer some protection against the progression of her disease.
View Answer
Answer and Discussion
The answer is c.
Objective: Manage HIV during pregnancy.
Two things are important about HIV during pregnancy: first, the management of HIV and HIV-related complications in the mother; and second, minimizing the risk of vertical transmission. The management of HIV and HIV-related complications is similar to the one recommended in the patients who are not pregnant, including the prophylaxis against opportunistic infections. As such, PCP prophylaxis should be initiated with a CD4 count of <200. Either trimethoprim/sulfamethoxazole or aerosolized pentamidine is used for PCP prophylaxis if indicated. Pregnancy does not affect the progression of the disease. In addition, HIV has no effect on the pregnancy course once social factors are controlled for.
The risk of transmission from the mother to the infant is believed to be related to the viral load. The risk of vertical transmission is as high as 33% of infants born to untreated mothers versus less than 7% in those infants born to mothers receiving perinatal antiviral medication.
The optimal timing and route of antivirals is debated, but most experts believe in treating with oral triple therapy (if
possible) from 14 weeks of gestation to delivery followed by intravenous (IV) therapy during labor and oral therapy to the infant for 6 weeks. If triple therapy is not possible, intrapartum zidovudine conveys the most benefit if given alone. If a mother is on antiretrovirals at the time of conception, they should be continued during the first trimester.
Question 19
All the following statements concerning rhinitis are true, except
a) An increased risk of allergic rhinitis exists if there is a family history of allergic rhinitis.
b) Eosinophils can be seen on Wright-stained nasal secretions.
c) Over-the-counter oral sympathomimetic agents may provide some relief of congestive symptoms, but they can cause elevation of BP and can be dangerous in patients with hypertension or in those at risk for cardiac events.
d) Nasal sympathomimetic agents are an excellent choice for the long-term symptom relief.
e) Hot and spicy foods may produce an episodic rhinitis termed gustatory rhinitis, which is a vagally mediated reflex.
View Answer
Answer and Discussion
The answer is d.
Objective: Understand key concepts about rhinitis.
Nasal sympathomimetic agents are not to be used for long-term symptom relief. Their use is limited to 2 to 3 days, to avoid the development of rhinitis medicamentosa. In rhinitis medicamentosa, rebound nasal congestion occurs after the discontinuation of a strong nasal decongestant, creating a vicious cycle, with the patient restarting the nasal spray to treat the congestion, which is directly caused by the nasal spray itself.
Question 20
A 28-year-old woman in her 20th week of gestation comes to the emergency department (ED) with shortness of breath.
She has had asthma since childhood that was previously well controlled. She stopped all medications because of concerns for the fetus. On examination, she appears to be in severe respiratory distress, with a respiratory rate (RR) of 28/minute. Her other vitals include a BP of 102/56 mmHg, pulse (P) of 100/minute, and 97% saturation on room air. Her lung examination is significant for wheezing in all lung fields. The rest of the examination is unremarkable. You diagnose her as having an exacerbation of asthma. Appropriate therapy might include all but
She has had asthma since childhood that was previously well controlled. She stopped all medications because of concerns for the fetus. On examination, she appears to be in severe respiratory distress, with a respiratory rate (RR) of 28/minute. Her other vitals include a BP of 102/56 mmHg, pulse (P) of 100/minute, and 97% saturation on room air. Her lung examination is significant for wheezing in all lung fields. The rest of the examination is unremarkable. You diagnose her as having an exacerbation of asthma. Appropriate therapy might include all but
a) Subcutaneous epinephrine
b) Inhaled metaproterenol
c) Oxygen by mask
d) Inhaled albuterol
e) IV steroids
View Answer
Answer and Discussion
The answer is a.
Objective: Identify the management of asthma during pregnancy.
Minimizing the known risks of maternal hypoxia to the fetus is preferred to minimizing the theoretical risks of medications. Therefore, encouraging compliance with medications is important. Almost all asthma medications are used safely during pregnancy. The exception is epinephrine, which can decrease the uterine perfusion. A better choice is terbutaline, 0.25 mg subcutaneously, which is often used to treat preterm labor.
Question 21
A 34-year-old diabetic woman is in her 10th week of gestation. Her diabetes was previously well controlled, but she has had problems maintaining her blood sugar control with recent changes in diet. She is also concerned about her risk of hypoglycemia. Her examination is unremarkable. You advise her that all of the following have been associated with poor glycemic control in diabetic women who become pregnant, except
a) Increased first-trimester miscarriages
b) Increased neural tube defects
c) Increased birth weight
d) Increased neonatal glucose levels
e) Increased neonatal respiratory distress syndrome
View Answer
Answer and Discussion
The answer is e.
Objective: Identify the risk of maternal diabetes to the fetus.
Insulin does not cross the placenta, but glucose does. The fetus will make its own insulin to respond to the high glucose levels. This leads to hypoglycemia after the umbilical cord is cut, as the glucose supply is interrupted. Both large-for-gestational-age and growth-restricted babies are born to diabetics, depending on the effect on the placenta, which is also an end organ like the kidneys and the eyes. Larger babies tend to have less mature lungs; the mechanism for this is unknown. Miscarriages and birth defects are more common in preexisting diabetics, as opposed to gestational diabetics.
Question 22
A 36-year-old woman with diabetes and hypertension has just found out that she is pregnant. Her BP has been well controlled with enalapril 10 mg daily. She has come for her annual primary care visit and has not yet seen an obstetrician. Her BP in your office is 136/78 mmHg. Which of the following medications is contraindicated for the treatment of hypertension in pregnancy?
a) Propranolol
b) Methyldopa
c) Hydralazine
d) Enalapril
e) Labetalol
View Answer
Answer and Discussion
The answer is d.
Objective: Identify antihypertensives safe during pregnancy.
Angiotensin-converting enzyme inhibitors (ACEIs) are associated with fetal compromise and death when exposure occurs during the second and third trimesters. ACEIs are considered class D medications during pregnancy, meaning that they have known teratogenic properties. Methyldopa is a class B medication during pregnancy, indicating that while there are no well-designed human trials, there are no teratogenic effects noted in animal models, and there is no anecdotal evidence of teratogenic effects in humans or there are teratogenic effects in animal models but not in human models. The rest of the medications above are considered class C medications, suggesting that either animal studies have shown risks and there are no human studies, or no animal or human studies have been conducted. Clinically, all the medications listed other than enalapril are used during pregnancy.
Question 23
A 26-year-old woman in her seventh month of pregnancy presents to the ED with increasing shortness of breath. She also complains of left leg swelling. She has no other medical problems and is not currently taking any prescription medications. On examination, she is in moderate respiratory distress. Her vital signs are as follows: RR = 28/minute, BP = 108/64 mmHg, P = 120/minute, and pulse oximetry = 89% on room air. Cardiac examination is significant for a regular, tachycardic rhythm; chest examination reveals no abnormalities; abdominal examination shows an enlarged uterus with palpable fetus; and extremities reveal left leg redness and swelling at the level of the calf. In addition to oxygen, what would be the most appropriate next step?
a) Doppler study of leg, then IV heparin if positive
b) Spiral CT, then weight-adjusted low molecular weight heparin (LMWH) subcutaneously if indicated
c) Ventilation-perfusion scan, then IV heparin if positive
d) IV heparin while awaiting radiographic studies
e) Doppler leg study and vena cava filter to prevent pulmonary embolism (PE) if positive
View Answer
Answer and Discussion
The answer is d.
Objective: Identify and manage Deep Vein Thrombosis/Pulmonary Embolism in pregnancy.
In patients with DVT/PE, early anticoagulation with heparin or LMWH decreases mortality. Also, the risk of DVT and PE is increased during pregnancy. Heparin does not cross the placenta and is easily reversed, so immediate anticoagulation carries little risk. Once that is done, do not hesitate to make the definitive diagnosis. Fetal risk from radiation is minimal compared with the risk of untreated DVT or PE, or ongoing anticoagulation without a documented diagnosis. Ventilation-perfusion scanning, spiral CT, angiography, and venography are all worth the risk. Long-term full anticoagulation with heparin or LMWH is preferred to warfarin. A filter is indicated only if anticoagulation cannot be safely accomplished.
Question 24
Assume that 20% of patients truly have disease X. Using a new test (X-ometry) to test 100 patients in your office for disease X, a total of 40 of these 100 patients are found to have positive X-ometry. The specificity of X-ometry is known to be 60%. What is the positive predictive value of positive X-ometry under these conditions?
a) 10%
b) 20%
c) 40%
d) 60%
View Answer
Answer and Discussion
The answer is b.
Objective: Calculate the positive predictive value given the sensitivity, specificity, and prevalence.
Complete the following table using the partial information provided:
| ||||||||||||||||||
The steps to calculate the positive predictive value are as follows:
Step 1. The example specifies a population prevalence of disease X of 20%. Thus, of 100 patients who are tested, 20 are expected to have the condition disease X—that is, the frequencies A and C add to 20.
Step 2. The problem specifies that 40 of the 100 patients tested have a positive test, so A + B is 40, and the other marginal values of the table can be determined by subtracting the known values from 100, which is the total number of patients examined in this example.
Step 3. The specificity of the test is designated to be 60%, so that 60% of the 80 patients without disease X in this example have a negative X-ometry test result. Frequency D is thus 60% of 80, or 48. The frequency in each of the other cells in this 2 × 2 table can then be specified.
Step 4. Once the cells are all filled in, it is possible to calculate the value of the positive predictive value of X-ometry in this example by calculating cell A (=8) divided by the sum of cells A + B (= 8 + 32, or 40). The correct answer for the positive predictive value is therefore 8/40, or 20%, in this example.
Question 25
Suppose that a screening mammography test for breast cancer has both high sensitivity and specificity, say 95% and 90%, respectively. What are the positive and negative predictive values of the test when applied to women with a 1% prevalence of breast cancer?
Positive predictive value is:
a) 0.514
b) 0.333
c) 0.154
d) 0.088
Negative predictive value is:
a) 0.999
b) 0.994
c) 0.989
d) 0.950
View Answer
Answer and Discussion
The answers are d and a.
Objective: Calculate the positive and negative predicative values given the sensitivity, specificity, and prevalence.
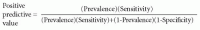
Bayes’ theorem can be applied to calculate the positive and negative predictive values given the specified values of sensitivity, specificity, and prevalence. The Bayes’ theorem for positive predictive value is generally calculated with the following equation:
The prevalence is 0.01, so the positive predictive value is (0.01)(0.95)/[(0.01)(0.95) + ((1 – 0.01) (1 – 0.90))], which equals 0.0095/(0.0095 + 0.099), or 0.088.
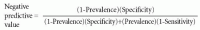
Likewise, the Bayes’ theorem for negative predictive value is generally calculated with the following equation:
Therefore, the negative predictive value is (1 – 0.01) (0.90)/[(1 – 0.01)(0.90) + (0.01)(1 – 0.95)], which equals 0.891/(0.891 + 0.0005), or 0.999.
Question 26
Using the same sensitivity and specificity as in question 25, what are the positive and negative predictive values of the test when applied to women with a 10% prevalence of breast cancer (e.g., those with a self-diagnosed lump in a breast)?
Positive predictive value is:
a) 0.667
b) 0.514
c) 0.333
d) 0.167
Negative predictive value is:
a) 0.994
b) 0.989
c) 0.950
d) 0.900
View Answer
Answer and Discussion
The answers are b and a.
Objective: Identify the effect of prevalence on the positive and negative predictive values.
The prevalence is 0.10, so the positive predictive value is (0.10)(0.95)/[(0.10)(0.95) + (1 – 0.10)(1 – 0.90)], which equals 0.095/(0.095 + 0.09), or 0.514. Likewise, the negative predictive value is (1 – 0.10)(0.90)/[(1 – 0.10)(0.90) + (0.10) (1 – 0.95)], which equals 0.810/(0.810 + 0.005), or 0.994.
Think about how the positive and negative predictive values changed when the prevalence increased from question 25 to question 26. If one were to hold the sensitivity and specificity of a test, increasing the prevalence of a disease will increase the positive predictive value and decrease the negative predictive value.
Question 27
In statistical hypothesis testing where the null hypothesis is like having no disease and the alternative hypothesis is like having disease, the statistical power of the hypothesis test is analogous to:
a) Sensitivity
b) Specificity
c) 1 – sensitivity
d) 1 – specificity
View Answer
Answer and Discussion
The answer is a.
Objective: Correlate statistical power to the sensitivity of a test.
In a statistical test, rejecting the null hypothesis given that it is truly false is called the power of the test. This is equivalent to having a diagnostic test reject the presence of “no disease” to conclude that there is disease. Hence, this is analogous to sensitivity, the probability that the diagnostic test indicates there is disease when in fact there is disease present. Likewise, in hypothesis testing, the type I error rate (i.e., significance level) of rejecting the null hypothesis when it is really true is analogous to 1 – specificity of a diagnostic test, the false-positive rate.
Question 28
The most common cause of visual decline in a patient with diabetes mellitus is
a) Macular edema
b) Proliferative diabetic retinopathy
c) Diabetic papillopathy
d) Tractional retinal detachment
View Answer
Answer and Discussion
The answer is a.
Objective: Identify macular edema as the most common cause of visual decline in diabetic patients.
In the Western Hemisphere, diabetic retinopathy is the leading cause of blindness in patients younger than 65 years. While all of these conditions are associated with diabetic retinopathy, the leading cause of irreversible vision loss in patients with diabetes is macular edema given the significantly higher prevalence of macular edema compared with these other conditions. Proliferative diabetic retinopathy is rare in the initial stages of the disease, but can be as high as 11% to 15% in the end stages of the disease. Even at this time, nonproliferative diabetic retinopathy is more common. The pathophysiology of visual loss in nonproliferative diabetic retinopathy is most commonly associated with macular edema.
Question 29
The most appropriate initial intervention for a patient with a corneal ulcer is
a) No treatment
b) Corneal cultures and sensitivities
c) Eye patch
d) Broad-spectrum topical antibiotics four times a day
View Answer
Answer and Discussion
The answer is b.
Objective: Identify and manage a corneal ulceration.
Most corneal ulcers are caused by infections. People who wear contact lenses are at an increased risk for corneal ulcers.
The risk of corneal ulcerations increases 10-fold when using extended-wear soft contact lenses. Patching is not indicated because it creates a warm, dark environment that allows bacterial growth. Once a pathogen has been identified, targeted antibiotic eye drops and oral pain medications are the mainstay of therapy.
The risk of corneal ulcerations increases 10-fold when using extended-wear soft contact lenses. Patching is not indicated because it creates a warm, dark environment that allows bacterial growth. Once a pathogen has been identified, targeted antibiotic eye drops and oral pain medications are the mainstay of therapy.
Question 30
The most common ocular manifestation in patients with rheumatoid arthritis is
a) Uveitis
b) Keratoconjunctivitis sicca
c) Conjunctivitis
d) Keratitis
View Answer
Answer and Discussion
The answer is b.
Objective: Identify ocular problems in rheumatoid arthritis.
The most common ocular problem in patients with rheumatoid arthritis is keratoconjunctivitis sicca or secondary Sjögren syndrome associated with connective tissue disease. Dry eyes occur in 11% to 13% of patients and this condition is characterized by lymphocytic infiltration of lacrimal and salivary glands with subsequent glandular destruction.
Scleritis is the second most common ocular finding, occurring in 1% to 6% of patients with rheumatoid arthritis. Posterior segment lesions due to rheumatoid arthritis are rare.
Question 31
In the Western Hemisphere, the leading cause of irreversible blindness in patients older than 65 years is
a) Cataract
b) Diabetic retinopathy
c) Glaucoma
d) Age-related macular degeneration (AMD)
View Answer
Answer and Discussion
The answer is d.
Objective: Identify the etiology of visual loss in elderly patients.
In the Western Hemisphere, diabetic retinopathy is the leading cause of blindness in patients younger than 65 years; AMD is the most common cause of irreversible blindness in patients older than 65 years. Macular degeneration affects up to 10% of patients between the ages of 65 and 75 years and up to 30% of patients between 75 and 85 years. There are two types of macular degeneration, dry type and wet type. Dry AMD accounts for up to 90% of cases of AMD. Patients will generally get a central visual field loss that is progressive over time.
Question 32
Which of the following is a known cause of retinal detachment?
a) Diabetes
b) Cataract surgery
c) Ocular trauma
d) Severe nearsightedness (long eyeballs)
e) All of the above
View Answer
Answer and Discussion
The answer is e.
Objective: Identify etiologies of retinal detachment.
Retinal detachment occurs when the lining of the eye comes off, thus causing loss of vision. Causes of retinal detachment include ocular trauma, posterior vitreous detachment, traction from an inflamed vitreous, long eyeballs (as in very nearsighted people), family predisposition, degenerative changes in the retina, complications from diabetes, and complications of intraocular surgery, including cataract surgery.
Question 33
You are asked to see a 54-year-old man for a preoperative evaluation prior to total hip arthroplasty. He has a 15-year history of non-insulin-dependent diabetes mellitus, chronic renal insufficiency, and hypertension. His medications include glyburide, metformin, and lisinopril. He has mild retinopathy and 300 mg/day of proteinuria. His last laboratory studies 2 weeks ago showed a creatinine of 2.1 mg/dL, total cholesterol of 256 mg/dL, high-density lipoprotein cholesterol 39 mg/dL, low-density lipoprotein cholesterol of 152 mg/dL, triglycerides of 210 mg/dL, and glycosylated hemoglobin of 7.2%. He has no past history of cardiovascular disease and denies current chest pain, palpitations, or dyspnea on exertion. For the past year, he has had limited physical activity due to progressive osteoarthritis of the hip. On examination, his weight is 220 lb with a body mass index of 32, BP 132/84 mmHg, and P 84/minute. His funduscopic examination shows mild background retinopathy. His cardiac and pulmonary examinations are normal, whereas the remainder of his examination is otherwise unremarkable except for mildly diminished dorsalis pedis pulses and a decreased position sense in his toes. His ECG shows nonspecific ST-T wave changes. Which of the following is the most appropriate preoperative recommendation at this time?
a) Ultrasound vascular evaluation of the lower extremities
b) Dobutamine stress echocardiography or dipyridamole thallium imaging
c) No further cardiac testing and proceed with surgery
d) Cardiac catheterization
View Answer
Answer and Discussion
The answer is b.
Objective: Identify indications for preoperative cardiac testing.
Using the American College of Cardiology and the American Heart Association (ACC/AHA) guidelines, this patient has several clinical risk predictors (h/o type 2 diabetes mellitus and chronic renal insufficiency) and is scheduled for an intermediate-risk surgery. Because his functional class is poor with
activity <4 metabolic equivalent of tasks (METs), he should undergo further risk stratification with noninvasive testing.
activity <4 metabolic equivalent of tasks (METs), he should undergo further risk stratification with noninvasive testing.
Once high risk features have been ruled out (active ischemia, decompensated congestive heart failure, and ventricular arrhythmia), patients going for intermediate-risk surgery should have their functional status assessed. If the patient is able to consistently undergo at least 4 METs of activity, then no further preoperative testing for cardiovascular disease is needed. However, this patient is not able to do 4 METs due to his osteoarthritis and has multiple (at least three) risk factors for coronary artery disease. With an abnormal baseline ECG, stress testing with an imaging modality may be indicated.
Question 34
You are asked to evaluate a 73-year-old man with stable class II angina treated with nitrates and atenolol, and no previous myocardial infarction or coronary heart failure. He has mild hypertension controlled with lisinopril and no history of diabetes. He had excellent exercise capacity (7 METs) until he injured his ankle 2 weeks ago. At that time, he was found to have a 5.2-cm abdominal aortic aneurysm. His examination is unremarkable, his BP is 144/86 mmHg, and his heart rate is 65/minute. His ECG is normal. He is scheduled to undergo abdominal aortic aneurysm repair. Which of the following is the most appropriate recommendation at this time?
a) Exercise stress test
b) Dobutamine stress echocardiography or dipyridamole thallium imaging
c) No further cardiac testing and proceed with surgery
d) Cardiac catheterization
View Answer
Answer and Discussion
The answer is c.
Objective: Identify indications for preoperative testing to assess for the cardiovascular risk.
Applying the ACC/AHA guidelines to this patient with chronic stable class II angina with excellent functional class would suggest that he did not undergo any further risk stratification with a stress test unless there would be a change in management.
This patient is able to consistently do >4 METs of activity and is safe to proceed to surgery. No further testing is indicated given his good functional capacity.
Question 35
A 48-year-old woman is referred for preoperative evaluation before a planned elective laparoscopic cholecystectomy. She has no prior cardiac history but has had asthma since age 16 years. Her current medications are oral theophylline and inhaled albuterol. She does not smoke and notes no dyspnea on moderate exertion. On examination, her weight is 97 kg (213.4 lb), height 163 cm (5′ 4″), BP 144/78 mmHg, and P 76/minute and regular. Her lungs reveal moderate wheezing that does not clear with cough. Her heart is normal, and, other than obesity, the remainder of her examination is normal. Which of the following is the most appropriate next step?
a) Add inhaled salbutamol before surgery
b) Add inhaled betamethasone before surgery
c) Reassure her that her risk is low because of the planned laparoscopic approach
d) Cancel the surgery and optimize antiasthma treatment regimen before rescheduling
View Answer
Answer and Discussion
The answer is d.
Objective: Manage perioperative pulmonary complaints.
The presence of active wheezing places this patient at greater risk for postoperative pulmonary complications and increased bronchospasm risk during anesthesia induction. The patient’s surgery should be delayed until her asthma treatment is optimized. The laparoscopic approach may reduce the risk of pulmonary complications compared with the open cholecystectomy, but a level of risk remains because of gaseous peritoneal distention and postoperative pain.
Question 36
A 27-year-old man is evaluated in the emergency room for the abrupt onset of neck pain associated with dizziness, slurred speech, and difficulty walking. He was in his usual state of health until 3 hours ago, when he developed the acute onset of posterior-lateral neck pain, shortly after he left an appointment with his chiropractor. Soon after, he noticed a sense of spinning and began slurring his words. He is unsteady when he walks, and within the last 30 minutes, he has had difficulty swallowing. His past medical history is negative except for occasional musculoskeletal complaints. He does not take any regular medications. He drinks alcohol socially and does not use tobacco. He is not married, and he works as a bank manager. His vital signs are as follows: T = 37.1°C, P = 81 beats/minute, RR = 22/minute, and BP = 126/81 mmHg. Head, eyes, ears, nose, and throat (HEENT) examination reveals left ptosis with anisocoria (left pupil smaller than the right). Nystagmus is present. The neck is supple but tender to palpation. There is no jugular venous distention (JVD), adenopathy, or bruits. Cardiopulmonary and abdominal examinations are normal. Neurologic examination demonstrates left-sided dysmetria and decreased pain and temperature sensation on the left side of the face and right side of the body. A chemistry profile, complete blood cell count, and coagulation studies are normal. CT scan of the head without contrast is normal. Which of the following is the most appropriate next step in the evaluation of this patient?
a) Carotid ultrasound
b) Lumbar puncture
c) Transcranial Dopplers
d) MRI/magnetic resonance angiography (MRA) of the brain and neck
e) Repeat CT scan of the head without contrast in 24 hours
View Answer
Answer and Discussion
The answer is d.
Objective: Recognize a posterior circulation stroke resulting from a traumatic vertebral artery dissection.
This patient has an ischemic stroke in the posterior-inferior cerebellar artery distribution. The normal CT scan rules out an intracerebral parenchymal hemorrhage. In a previously healthy young person, less common causes of stroke such as vertebral artery dissection should be considered. Vertebral artery dissection often occurs suddenly with or without trauma. Manipulation by chiropractors has been associated with vertebral artery dissection. Symptoms can include neck or posterior head pain, Horner syndrome (ptosis and miosis), dysarthria, dysphagia, decreased pain and temperature sensation of the face and contralateral body, dysmetria, ataxia, and vertigo. MRA is the best choice to diagnose dissection in this patient. Repeat CT scan will show the evolving stroke but not the cause. Carotid ultrasound and transcranial Dopplers do not reliably characterize vertebral artery abnormalities. Lumbar puncture is indicated to evaluate subarachnoid hemorrhage in the setting of a normal CT scan; however, his neurologic examination with localized medullary symptoms would be very uncommon for a subarachnoid bleed.
Question 37
A 55-year-old man was brought to the ED via squad. His wife called 911 after the patient awoke this morning with a posterior headache, dizziness, and unsteady gait. His past medical history is significant for hypertension and known coronary artery disease. His medications include a baby aspirin, metoprolol, atorvastatin, and clonidine. He was not able to take his medications before arrival. In the emergency room upon presentation, he was awake, alert, and afebrile. He described severe vertigo. Vital signs were as follows: P = 65 beats/minute, RR = 24/minute, and BP = 175/97 mmHg. His HEENT examination revealed bidirectional nystagmus. His lungs were clear. Cardiac examination displayed normal heart tones with a +S4 gallop. Abdominal examination was normal. Neurologic testing revealed gait ataxia but normal muscle strength. Laboratory tests were unremarkable, and the CT scan of the head without contrast was normal. He was admitted for further observation, and examination several hours later revealed lethargy alternating with agitation, intractable hiccups, bidirectional nystagmus, and dysmetria of the right upper and lower extremities. Which of the following is the most likely diagnosis?
a) Vestibular neuronitis
b) Cerebellar infarction
c) Benign positional vertigo
d) Vestibular migraine
e) Ménière disease
View Answer
Answer and Discussion
The answer is b.
Objective: Recognize symptoms concerning for cerebellar stroke.
This patient presents with headache, vertigo, and ataxia, which are the classic presenting symptoms of ischemic or hemorrhagic cerebellar stroke. Although CT scan can exclude hemorrhage, infarcts may not be well visualized early, especially in the brainstem and cerebellum. The patient’s deterioration the following day, with signs of brainstem compression (altered level of consciousness and intractable hiccups), indicates a dire situation, and urgent neurosurgical decompression is required. Peripheral vertigo may be a result of many disorders of the ear, including vestibular neuronitis, benign positional vertigo, vestibular migraine, acoustic neuroma, and Ménière disease, but none of these causes limb ataxia, dysarthria, or hiccups. Headache may accompany vestibular migraine but is not a feature of the other peripheral disorders.
Question 38
A 35-year-old man is referred to you for preoperative evaluation prior to an inguinal hernia repair. He has no prior cardiac history and does not smoke or drink. On examination, he weighs 80 kg (176 lb), BP 140/80 mmHg, and P 80/minute. His heart and lungs, as well as the remainder of his examination, are normal. You recommend which of the following?
a) Complete metabolic profile
b) Complete blood count
c) Urine analysis
d) All of the above
e) None of the above
View Answer
Answer and Discussion
The answer is e.
Objective: Identify the preoperative testing in a healthy individual.
This patient is completely healthy, and the evidence would suggest that ordering routine preoperative blood work would be both unnecessary and costly, and not indicated in this patient’s case. A screening urine analysis is never indicated unless symptoms suggest that the patient may have an underlying infection.
Question 39
A 50-year-old woman with a 20-year history of rheumatoid arthritis is scheduled for a spine surgery. Her medications include prednisone 10 mg/day orally for the past year, vitamin E, gingko biloba, garlic, and aspirin. Her functional class is limited, but she can still climb a flight of stairs with her groceries (>4 METs). She denies any history of chest pain, shortness of breath, and prior cardiac problems. Her examination reveals a weight of 60 kg and height of 5′ 5″, BP of 120/70 mmHg, and heart rate of 80/minute. Heart and lung examinations are normal. Her neck examination reveals a decreased range of motion, and her extremities reveal deformities consistent with rheumatoid arthritis. Which of the following is the most appropriate recommendation?
a) Discontinue vitamin E, gingko biloba, and garlic
b) Discontinue aspirin 10 days before surgery
c) Obtain cervical spine films
d) Stress-dose steroids
e) All of the above
View Answer
Answer and Discussion
The answer is e.
Objective: Manage medications perioperatively.
The current evidence and consensus would support discontinuing vitamin E, ginkgo, and garlic about 2 weeks prior to surgery because they may all increase the risk of bleeding. Aspirin irreversibly inhibits the platelet cyclooxygenase and should be stopped 7 to 10 days before surgery. Cervical spine films are indicated in patients with rheumatoid arthritis before they undergo general anesthesia because the presence of severe atlantoaxial disease can cause a compromise of the cervical cord during manipulation of the neck during intubation; however, there is no role for further spine imaging. Although the risk of perioperative adrenal insufficiency is low, it is potentially catastrophic. Stress-dose steroids would be recommended to prevent this.
Question 40
A previously well 78-year-old man is admitted to the hospital for the treatment of a community-acquired pneumonia. The nurses report that he is sometimes hard to arouse, quiet, and withdrawn, while at other times he is agitated, disoriented, and accusatory, and behaves inappropriately. Physical examination is unremarkable except for the findings of pneumonia. Which of the following is the most accurate statement about his mental status?
a) He has dementia with “sundowning.”
b) The symptoms are potentially preventable.
c) A head CT scan is needed.
d) He has the “pseudodementia” of depression.
View Answer
Answer and Discussion
The answer is b.
Objective: Identify and manage delirium in an elderly hospitalized patient.
The acute onset of the change in mental status, the fluctuating course, and the altered level of consciousness are diagnostic of delirium. Although the cognitive dysfunction at night in a new environment (sundowning) can occur in patients with either dementia or delirium, the patient does not have a history of dementia, in which symptoms usually progress over a duration of months to years, and attention and level of consciousness are normal. A head CT scan is rarely useful in the diagnostic evaluation of a patient with delirium and is reserved for patients with new or focal neurologic signs or suspected head trauma. Patients with major depressive disorder often have cognitive dysfunction (“pseudodementia”), but are alert and attentive and do not have a fluctuating course. A clinical trial with hospitalized elderly patients demonstrated a 40% decrease in the incidence of delirium with an intervention that targeted the risk factors for delirium (cognitive impairment, sleep deprivation, immobility, visual and hearing impairment, and dehydration); the total number of days with delirium was also reduced by the intervention.
Question 41
A 77-year-old man has a 6-month history of frequent fallings. Because he loses his balance while walking, he is walking less and has a fear of falling. He takes a diuretic for hypertension and a nitrate for angina pectoris. On physical examination, he takes small, short steps, and has postural instability and decreased steppage. Routine blood test results are normal. The treatment most likely to reduce this patient’s risk of falling is
a) Change in medications
b) Gait training
c) Low-intensity resistive exercises
d) All of the above
e) None of the above
View Answer
Answer and Discussion
The answer is d.
Objective: Manage elderly patients with recurrent falls.
Recurrent falls occur in patients with disorders of balance and gait, lower extremity weakness (often from muscular deconditioning or atrophy), polypharmacy, and fear of falling. Drugs with cardiovascular (e.g., α-adrenergic blockers and vasodilators) or central nervous system (e.g., benzodiazepines) effects may worsen the postural stability or balance, increasing the risk of falling. Clinical trials provide strong evidence that balance and gait training, low-intensity resistive exercise (e.g., with weights, bands, or tubes), walking, or Tai Chi exercises can reduce the incidence of falls.
Question 42
A 68-year-old man presents in the office with a 3-day history of urinary urgency, dysuria, two episodes of large-volume urinary incontinence, and difficulty initiating urination. His examination is unremarkable. A urinalysis is positive for pyuria, nitrites, and trace proteins, but no glucose. A postvoid residual urine (by bladder scan) = 40 mL. His past medical history is only significant for benign prostatic hyperplasia, mild hypertension controlled with diet, and osteoarthritis of the knees. The treatment most likely to relieve his urinary incontinence is
a) Transurethral resection of the prostate
b) Antibiotics
c) α-Blocker (e.g., doxazosin)
d) Bladder relaxant (e.g., tolterodine)
e) Cholinergic agent (e.g., bethanechol)
View Answer
Answer and Discussion
The answer is b.
Objective: Manage the urinary incontinence in the elderly.
The patient has a urinary tract infection and is likely to respond to an antibiotic that will reduce his lower urinary tract symptoms
as well. Acute causes of urinary incontinence can be recalled by the pneumonic DRIP: Delirium, Restricted mobility, Impaction or Iatrogenic (physical restraints and excessive IV fluids) or Infection, Polyuria (glucosuria, loop diuretics, and anticholinergics), or Pharmaceuticals. The transurethral resection of prostate is indicated for men with severe lower urinary tract symptoms and/or bladder outlet obstruction unrelieved by medications, but this patient’s symptoms are acute and not associated with a large postvoid residual urine. An α-adrenergic blocker is often effective in reducing the irritative and obstructive symptoms of benign prostatic hyperplasia, but the patient did not have a history of chronic symptoms and an improvement with these medications might not be seen for several days or weeks. A bladder relaxant might reduce the intensity of the urinary urgency but would not eliminate the infection. A cholinergic agent would not eradicate the infection and might exacerbate the urge symptoms because it increases the detrusor muscle contractions.
as well. Acute causes of urinary incontinence can be recalled by the pneumonic DRIP: Delirium, Restricted mobility, Impaction or Iatrogenic (physical restraints and excessive IV fluids) or Infection, Polyuria (glucosuria, loop diuretics, and anticholinergics), or Pharmaceuticals. The transurethral resection of prostate is indicated for men with severe lower urinary tract symptoms and/or bladder outlet obstruction unrelieved by medications, but this patient’s symptoms are acute and not associated with a large postvoid residual urine. An α-adrenergic blocker is often effective in reducing the irritative and obstructive symptoms of benign prostatic hyperplasia, but the patient did not have a history of chronic symptoms and an improvement with these medications might not be seen for several days or weeks. A bladder relaxant might reduce the intensity of the urinary urgency but would not eliminate the infection. A cholinergic agent would not eradicate the infection and might exacerbate the urge symptoms because it increases the detrusor muscle contractions.
Question 43
An 84-year-old man is recovering from an abdominal surgery in the hospital. Four days after surgery, he attempts to get out of bed for the first time. He feels light-headed and unsteady and falls without an injury. He is now afraid to walk. Before the operation, he walked normally. He is taking a cardioselective α-blocker, a statin, and acetaminophen. Physical examination reveals normal cognition and vital signs and generalized weakness. He appears worried. Laboratory studies are unremarkable. Which of the following is most likely to improve his symptoms?
a) A β-blocker with intrinsic sympathomimetic activity rather than the cardioselective agent
b) Low-intensity resistive exercises for his lower extremities
c) A low dose of a psychostimulant (e.g., methylphenidate)
d) A four-prong cane
e) A benzodiazepine (e.g., lorazepam) to treat anxiety
View Answer
Answer and Discussion
The answer is b.
Objective: Identify and manage deconditioning in an elderly patient.
The patient probably has deconditioning associated with major surgery and prolonged immobility. With prolonged bed rest, a generalized weakness of the extensor and flexor muscles of the knees and hip muscles is common. Low-intensity exercises, active resistance against flexion or extension, and therapeutic bands or tubes increase muscle strength and lessen the chance of a fall. A β-blocker with intrinsic sympathomimetic activity could cause orthostatic hypotension and more light-headedness. A psychostimulant might be considered for a patient with depression and delayed recovery from surgery but would not increase the muscle strength. A four-prong cane is helpful when patients have weakness in one extremity, but is not indicated for patients with generalized weakness due to deconditioning. An anxiolytic could cause gait impairment and increase the risk of a fall.
Question 44
A 71-year-old woman presents with an 8-month history of urinary urgency, frequency, and nocturia, and daily urinary incontinence. Her past medical history is significant for occasional “stress incontinence” (with sneezing, coughing, and straining) for 12 years. She takes no daily medications. Physical examination reveals slight anterior vaginal prolapse and no visible leakage or pelvic mass. A screening urinalysis and basic metabolic panel are normal. Which of the following is most likely to relieve her urinary incontinence?
a) Bladder relaxant (oxybutynin)
b) Topical (vaginal) estrogen
c) α-Agonist (pseudoephedrine)
d) Behavioral therapies
e) Periurethral injections (collagen)
View Answer
Answer and Discussion
The answer is d.
Objective: Identify and manage mixed urinary incontinence.
The patient has mixed stress and urge incontinence. The stress incontinence is most likely a result of urethral hypermobility, whereas the urge incontinence likely represents an overactive bladder. Although bladder relaxants alone reduce the frequency of incontinent episodes due to urge incontinence, they have little or no effect on stress incontinence. Behavioral therapies (training), including pelvic floor exercise, pelvic floor stimulation, and biofeedback, are more effective than placebo or bladder muscle relaxants for mixed forms of incontinence. In one study, biofeedback to teach pelvic floor muscle control, verbal feedback based on vaginal palpation, and a self-help booklet in a first-line behavioral training program all achieved comparable improvements in urge incontinence in communitydwelling older women. Periurethral injections with bulking agents (collagen) are indicated for intrinsic sphincter deficiency (ISD) and have no effect on urge incontinence. The α-agonists and vaginal estrogen are of questionable value in the treatment of stress incontinence and have no proven effect in women with ISD.
Question 45
A 20-year-old man presents to the ED with altered mental status, diaphoresis, urinary incontinence, and shortness of breath. He is agitated, has pinpoint pupils, as well as diffuse wheezing. Family reports that he is a college student, and does odd jobs on the side to help make some additional money. Most recently, he had been working for a landscaping company and tutoring fellow students. The appropriate management of this patient includes all of the following, except
a) Atropine
b) Sodium nitrite
c) Pralidoxime chloride (Protopam)
d) Maintenance of airway
e) Decontamination
View Answer
Answer and Discussion
The answer is b.
Objective: Identify and manage organophosphate poisoning.
This patient has organophosphate poisoning as evidenced by his muscarinic and nicotinic overactivation, which may include altered mental status, diaphoresis, lacrimation, miosis, urination, defecation, bradycardia, and diffuse wheezing. Atropine blocks the muscarinic effects of organophosphates and should be administered promptly. Pralidoxime chloride (Protopam) reactivates the enzyme cholinesterase by breaking the acetylcholinesterase-phosphate complex. Its advantages over atropine include its ability to reverse muscle paralysis and possibly central nervous system depression.
Decontamination procedures may include removal of contaminated clothing, washing of skin and hair, and, if indicated by route of exposure, emptying the stomach. In severe cases, a patent airway needs to be established for the removal of excess secretions and institution of ventilatory support.
Sodium nitrite is used in cyanide poisoning. It has no role in the management of organophosphate toxicity.
Question 46
Which of the following side effects is most commonly seen with selective serotonin reuptake inhibitors (SSRIs)?
a) Weight gain
b) Sexual dysfunction
c) Sedation
d) QTc prolongation
e) None of the above
View Answer
Answer and Discussion
The answer is b.
Objective: Identify the side effects from SSRIs.
SSRIs are the most often prescribed medication class in depression. While a relatively safe and effective medication class, they are associated with some side effects. Sexual dysfunction is a very common side effect. Patients taking SSRIs (fluoxetine, sertraline, paroxetine, citalopram, and escitalopram) are more likely to report sexual dysfunction than those taking other agents such as bupropion and mirtazapine. The other side effects, notably weight gain and sedation, have been associated with many SSRIs, but not nearly as frequently as sexual dysfunction. QTc prolongation, while reported, is very rare and should often prompt investigation of other medications.
Question 47
Which of the following statements about somatic symptom disorders is correct?
a) There is a history of many physical complaints beginning before age 30 years.
b) When a related general medical condition exists, physical complaints are in excess of what would be expected.
c) These disorders respond better when the intervention is early, without reinforcement by the excessive ordering of tests and evaluations.
d) Patients should be told that the symptoms are “real” but not life-threatening.
e) All of the above
View Answer
Answer and Discussion
The answer is e.
Objective: Identify and manage somatic symptom disorders.
The Diagnostic and Statistical Manual of Mental Disorders criteria include finding a history of many physical complaints beginning before age 30 years that occur over a period of several years and result in a treatment being sought or a significant impairment in the social, occupational, or other area of functioning.
Treating the patient with short but regularly scheduled visits; reassurance; referral to a psychoeducational group, if available, to enhance optimal health; ordering only “necessary” testing; and treating comorbid psychiatric disorders, such as depression, are the cornerstones of managing these cases.
Question 48
Which of the following is not a characteristic feature of a panic attack?
a) Chest pain
b) Feeling dizzy
c) Diarrhea
d) Paresthesias
e) Sweating
View Answer
Answer and Discussion
The answer is c.
Objective: Identify symptoms that associate with panic attacks.
Panic attacks are characterized by intense fear triggering many somatic symptoms when no apparent threat is present. Panic attacks are very debilitating and while most individuals tend to only have one or two, the fear of having recurrent panic attacks can be crippling. Symptoms of panic attacks are generally quick in onset and can mimic a hyperadrenergic state, including chest pain, palpitations, light-headedness, dizziness, shortness of breath, nausea, difficulty swallowing, and paresthesias. Diarrhea is not a characteristic feature of panic attacks and should prompt an investigation of an alternative or concurrent diagnosis. Nausea and abdominal distress may be seen.
Question 49
Which of the following medications increases the risk of lithium toxicity?
a) Enalapril
b) Hydrochlorothiazide
c) Ibuprofen
d) Losartan
e) All the above
View Answer
Answer and Discussion
The answer is e.
Objective: Identify drug-drug interactions that affect renal clearance.
Lithium has renal clearance and is not hepatically metabolized. Therefore, any medications that alter sodium excretion and subsequently lithium excretion should be used with caution (e.g., diuretics, ACEIs, and nonsteroidal anti-inflammatory
drugs) because lithium levels may increase to the point of toxicity in only several days.
Question 50
A 56-year-old man is transferred from the intensive care unit (ICU) to the general medicine ward for a severe urinary tract infection. He is being treated with ciprofloxacin for this urinary tract infection and seems to be improving. He is not requiring ventilatory or vasopressor support. Overnight, he has an acute change in mental status and becomes agitated. He is not on any narcotics, benzodiazepines, antihistamines, anticholinergics, or sleep aides. His repeat lab work, including electrolytes, is within normal range. The nurse asks for some haloperidol, as this is what he would get in the ICU when he was agitated. Which of the following should be obtained before initiating haloperidol?
a) Thyroid-stimulating hormone
b) Hematocrit
c) ECG
d) Liver function tests
e) All of the above
View Answer
Answer and Discussion
The answer is c.
Objective: Identify the risk of QTc prolongation with haloperidol.
Haloperidol may alter the cardiac conduction and prolong QT Interval; life-threatening arrhythmias have occurred with therapeutic doses of antipsychotics, but the risk may be increased with doses exceeding recommendations and/or with IV administration (unlabeled route). Haloperidol should be used with caution or avoided in patients with electrolyte abnormalities (e.g., hypokalemia and hypomagnesemia), hypothyroidism, familial long QT syndrome, concomitant medications that may augment QT prolongation, or any underlying cardiac abnormality that may also potentiate the risk.
Question 51
A thin, 21-year-old white woman presents to the ED with an acute onset of shortness of breath. The examination is consistent with a pneumothorax. Chest radiography confirms this finding, along with evidence of mild hyperinflation and ring shadows in the upper lobes. She states that she was adopted and grew up in foster homes, noting that she was a “sickly” child with many episodes of sinusitis and bronchitis, and that lately she cannot get rid of a productive cough. Genetic testing reveals a mutation in the CF transmembrane conductance regulator (CFTR) gene on chromosome 7. Which of the following statements regarding this patient’s condition is false?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





