(1)
Department of Vascular Surgery, Evangelisches Krankenhaus Königin Elisabeth Herzberge, Berlin, Germany
An AV vascular access undergoes morphologic and functional changes. These may exert local or systemic influences on the whole organism and entail serious complications. Most complications are not unexpected but may be anticipated much earlier. Therefore continuous monitoring during dialysis treatment is advisable. For this purpose no undue extra effort is necessary.
18.1 History
The patient should explicitly be asked for the following complaints and be examined for the following abnormalities:
Pain of the extremity distal to the AV anastomosis (reduced peripheral perfusion?)
Edema of the shunt extremity (venous congestion?)
Exercise-induced dyspnoea or palpitations (cardiac strain due to shunt flow?)
Fatigue/vertigo with AV accesses of the upper extremity (occlusion of the subclavian artery with subclavian steal syndrome?)
Signs of pathologic recirculation/ineffective dialysis
18.2 Inspection
The inspection of a vascular access and its surroundings does not require any relevant additional time. The following particularities are of special interest:
Edema (lymphatic? venous congestion? perigraft seroma?)
Inflammatory erythema (infection?)
Dilated veins central to the AV access (central venous stenosis?)
Bright red reticular veins (retrograde venous arterialization?)
Pallor distal to the AV anastomosis (reduced peripheral perfusion? capillary refill?)
Aneurysms
State of puncture sites
18.3 Palpation
Palpation allows for statements on:
Function of an AV access
Vascular morphology
Palpation helps evaluate:
Character of the thrill
Pulsatility
Pressure
Based on these findings, the flow rate, the arterial inflow, and the venous outflow may be determined qualitatively.
The thrill originates in the anastomosis and in the adjacent segment of the AV vessel. It is caused by high frequency vorteces. Pressure changes are transmitted along the vascular wall. The thrill occurs when there is inflow of blood under high pressure (artery) into a wide-lumen low pressure vessel (vein or prosthesis). The higher the absolute blood pressure and the pressure gradients, the more pronounced the thrill. There is also a superposition of the pulsatile flow. Frequency and amplitude influence the thrill. The intensity of the thrill decreases with the distance from the AV anastomosis. Often the thrill is also transmitted into the feeding artery. This phenomenon can be observed distally more often than proximally. The following palpation technique has proven useful: The long fingers II–IV are gently placed side by side on the vessel. Thus a two-dimensional impression of the flow character may be gained.
18.3.1 Findings on Palpation for Flow Evaluation
Optimal Flow Characteristics
Conditions: sufficient inflow and outflow.
Palpation (Fig. 18.1a): strong, pulse-synchronous thrill.


Fig. 18.1
Findings on palpation. (a) Optimal flow characteristics. (b) Low arterial inflow. (c) Disturbed venous outflow
Insufficient Arterial Inflow
Conditions: insufficient arterial inflow, low venous outflow resistance:
Central arterial stenosis?
Narrow feeding artery?
Narrow anastomosis?
Hypotension?
Palpation (Fig. 18.1b): attenuated, exclusively systolic thrill with low pulsatility
Insufficient Venous Outflow
Conditions: sufficient arterial inflow, high venous outflow resistance:
Stenosis of the efferent vein?
Central venous stenosis?
Stenosis of the venous anastomosis with AV prosthetic grafts?
Palpation (Fig. 18.1c): strong pulsation with discrete systolic thrill
Stenosis Along the AV Access
Conditions: sufficient arterial inflow, low venous outflow resistance, stenosis of the AV vessel.
Palpation:
Get Clinical Tree app for offline access

Upstream from the stenosis: strong pulsations with low systolic thrill
Stenosis: strong pulsation without thrill
Downstream from the stenosis: strong pulse-synchronous thrill with attenuated pulse (Fig. 18.2)
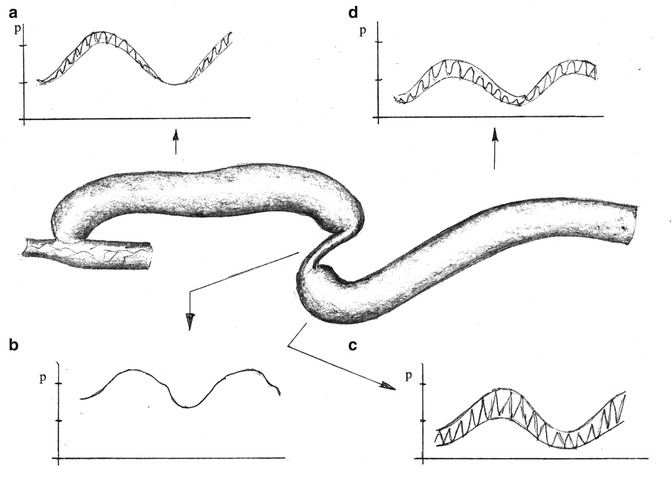
Fig. 18.2
Findings on palpation with stenosis in the AV vessel. (a) Pulsations with only slight systolic thrill. (b) Strong pulsations without thrill. (c) Strong thrill in sync with the pulsations. (d) Decrease of the thrill with increasing distance
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








