Chapter 1 Minimally Invasive Video-Assisted Thyroidectomy
Operative indications
The inclusion criteria and the main contraindications for MIVAT are summarized in Table 1-1. The main limiting factor is the size of both the nodule and the thyroid gland, as measured by preoperative ultrasonography. In geographic areas with endemic goiter, the gland volume can vary considerably compared with the nodule volume. Thus, if the gland was not adequately imaged before attempting MIVAT, there is increased risk for conversion to open thyroidectomy. Ultrasonography also may be useful to exclude thyroiditis, which can increase the difficulty of the dissection. If thyroiditis is suspected by ultrasonography, then serum autoantibodies should be determined. In general, thyroiditis by itself should not be an indication for MIVAT.
Table 1-1 Indications and Contraindications for MIVAT
| Indications | Contraindications |
|---|---|
| Benign disease* | Recurrent disease |
| Low risk papillary carcinoma Graves disease | Locally advanced and/or metastatic carcinoma Short neck in an obese patient |
* Thyroid volume less than 25 mL and nodule diameter less than 3 cm.
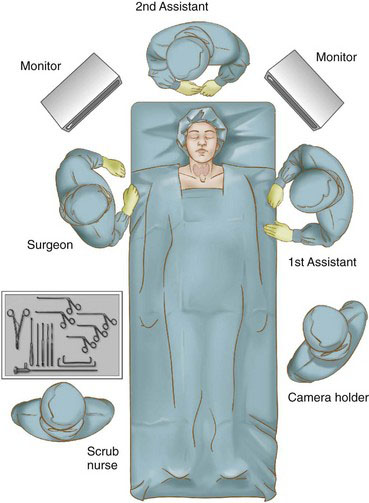
Patient positioning
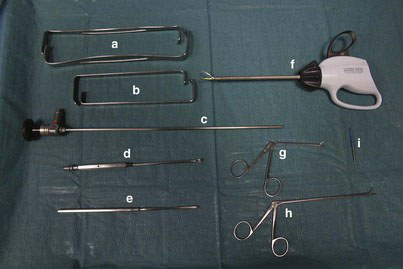
The operation is performed with the patient under general anesthesia; alternatively, a deep bilateral cervical block may be used. The patient is placed supine without neck hyperextension (Fig. 1-1). After aseptic preparation, the skin is protected with a transparent adhesive film (e.g., Tegaderm, 3M, St. Paul, Minn.) and then draped. The surgeon stands on the patient’s right, the first assistant is opposite the surgeon on the left, the second assistant is at the head of the table, the camera operator is on the patient’s left and caudal to the first assistant, and the scrub technician is on the right and caudal to the surgeon (Fig. 1-2). Two monitors, one facing the surgeon and the other facing the first assistant, are optimum. The basic instrumentation used for MIVAT is shown in Figure 1-3. Other helpful instruments include a suction dissector, thin ear forceps, vascular clip applier, and straight scissors.
Operative technique
Preparation of the Operative Space
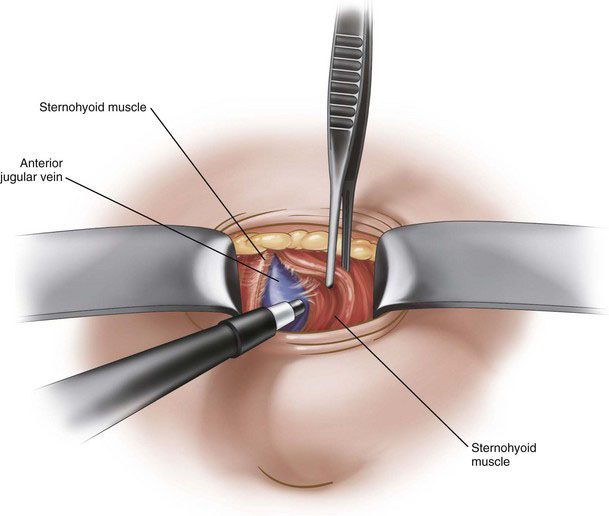
A 1.5-cm horizontal skin incision is performed 2 cm above the sternal notch. Subcutaneous fat and platysma are carefully dissected to minimize bleeding. During this step of the procedure, the use of the insulated electrocautery blade (see Fig. 1-3) is preferred to avoid damage to the skin and the superficial planes. Two small retractors are used to expose the deep cervical fascia, which is incised in the vertical midline in a bloodless plane for 2 to 3 cm (Fig. 1-4). The thyroid lobe is then bluntly dissected from the strap muscles using small spatulas (see Fig. 1-3) and gentle retraction. When the thyroid lobe is almost completely dissected from the strap muscles, larger double-ended retractors (Army-Navy type; see Fig. 1-3) can be inserted to maintain the operative space during the endoscopic portion of the procedure (Fig. 1-5). A 30-degree, 5-mm (or 7-mm) endoscope is then introduced through the skin incision to commence the endoscopic portion of the procedure (Fig. 1-6).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree