Chapter 34 Minimally Invasive Retroperitoneal Adrenalectomy
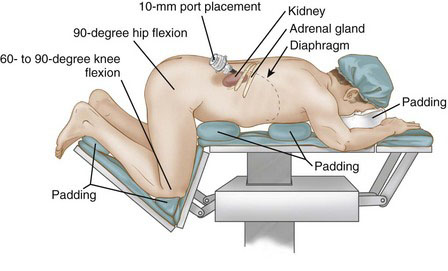
Patient positioning in the operating suite
Retroperitoneoscopic adrenalectomy is performed with the patient in the prone jackknife position, as shown in Figure 34-1. The upper extremities are flexed at the elbows and pronated. The hips and knees are flexed at a 60- to 90-degree angle. It is important to flex the hips to expose the area between the posterior costal margin and the iliac crest and to permit adequate space for port placement. All pressure points, including the chest, hips, and knees, should be padded. The torso of the patient is kept parallel to the floor.
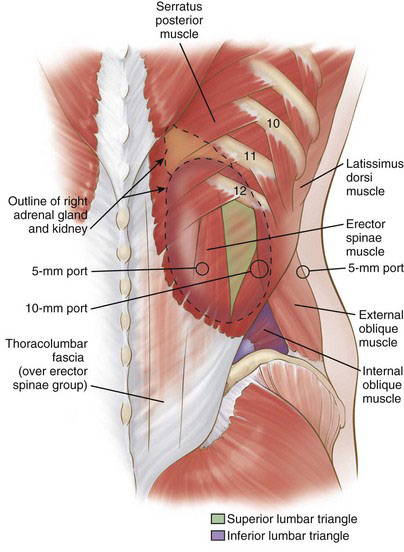
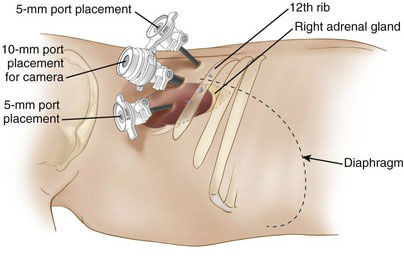
Positioning and placement of trocars
Posterior retroperitoneoscopic adrenalectomy can be performed using either a three-port or a single-port technique. With the three-port approach, the first (10-mm) trocar is placed 1 fingerbreadth below the tip of the 12th rib (Fig. 34-2). If fascia is encountered instead of muscle fibers, then it likely is the thoracodorsal (lumbodorsal) fascia, which invests the erector spinae muscles, meaning that the incision was too medial. If the thoracodorsal fascia is identified and the trocar is passed just lateral to this landmark, then the superior lumbar triangle likely will be traversed (see Fig. 34-2). The musculofascial layers in the region of the triangle are, from superficial to deep, the latissimus dorsi muscle, external oblique muscle, and transversalis fascia (Fig. 34-3). The superior lumbar triangle is the thinnest point of the posterior abdominal wall and is a potential location for incisional hernia. Ideally, therefore, the initial trocar should traverse lateral to this triangle. It often is difficult to ascertain the borders of this triangle, so this 10-mm port site should be closed securely at the procedure’s conclusion.
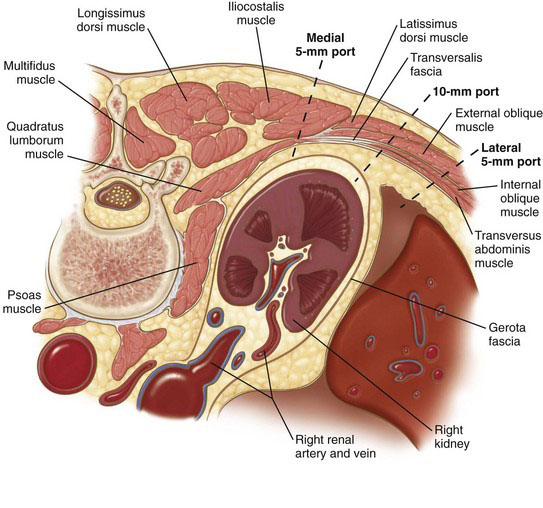
FIGURE 34-3 Transverse section of abdomen showing layers of posterior abdominal wall traversed by the ports in Figure 34-2.
A properly placed 10-mm port-site incision should sequentially go through skin, subcutaneous fat, external oblique muscle, internal oblique muscle, transversus abdominis muscle, and transversalis fascia before reaching the retroperitoneal space (see Fig. 34-3). If the port is placed slightly cephalad and medial, then the surgeon will sequentially encounter skin, subcutaneous fat, tail of latissimus dorsi overlying the external oblique, external oblique, internal oblique, transversus abdominis, and transversalis fascia. Penetration through the transversalis fascia yields entry into the retroperitoneum, in particular the posterior pararenal space (see Fig. 34-2). Finger dissection can be performed through the port incision to increase the retroperitoneal working space. The 10-mm port then can be placed, followed by a 30-degree laparoscope; the latter can be used to bluntly dissect additional working space. Alternatively, a balloon dissector can be used to establish this space.
After a working space has been established, carbon dioxide is insufflated to a pressure of 20 to 25 mm Hg. Two additional 5-mm ports then are placed under laparoscopic visualization (see Fig. 34-2). The first is placed medial to the 10-mm port but lateral to the erector spinae muscles. Port traversal through the paraspinous muscles should be avoided because it is difficult to enter the working space and subsequently maneuver the port through this muscle mass. The second 5-mm port is placed lateral to the 10-mm port. The three ports should be aligned horizontally and spaced at least 3 cm apart to prevent interference (Fig. 34-4). The central (10-mm) port typically is used for the laparoscope. If a different dissection angle is desired, however, then a 5-mm laparoscope can be used through the medial or lateral port so that the working ports can be switched.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree