Chapter 33 Minimally Invasive Radical Prostatectomy
Patient positioning and operative room setup
For standard LRP, the legs remain in the supine position and are secured to the bed with a safety strap. With RARP, the legs are placed in low lithotomy position with Yellowfins stirrups (Allen Medical Systems, Acton, Mass.), taking care not to place excessive strain on the thigh or groin muscles, which can produce postoperative neurapraxia. Alternatively, a spread-leg position (using spreader bars designed for the table) can be used with the patient in supine position. An overview of the patient positioning is shown in Figure 33-1.
Positioning and placement of trocars
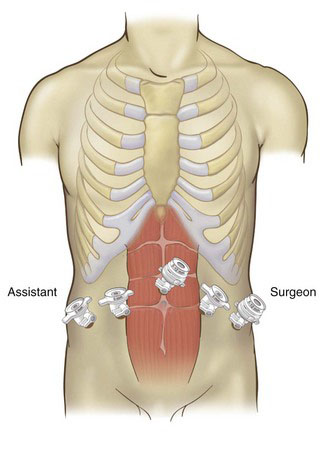
For MIRP, a fan-shaped configuration of trocars in the lower abdomen is used (Fig. 33-2). Five trocars are used during LRP, and six trocars are placed for RARP. A Foley catheter is inserted in a sterile fashion on the field, and the bladder is emptied. Bulb suction is preferred to ensure that the bladder remains empty during the early dissection. After gaining access to the peritoneal cavity, a 12-mm blunt trocar is placed in a supraumbilical midline location for the laparoscope in both types of MIRP. The bed then is placed into Trendelenburg position (13 to 15 degrees, head down).
For standard LRP, a 12-mm trocar is placed 2 fingerbreadths from the left anterior superior iliac spine (ASIS) on a line from the ASIS to the umbilicus (see Fig. 33-2). This trocar is used by the surgeon to pass suture into the abdomen throughout the procedure and for the surgeon’s grasper during dissection. A 5-mm trocar is placed along this line in the left lower quadrant at the lateral border of the left rectus muscle. The ultrasonic scalpel is used through this trocar during the dissection. Two additional 5-mm trocars are placed in a mirror image in the right lower quadrant for the assistant to use for the suction irrigator and retraction during the procedure. The authors prefer to use low-profile trocars during standard LRP to allow for maximal instrument reach into the pelvis.
For RARP, a similar port configuration is used (Fig. 33-3). Two robot ports are placed in the left lower quadrant as described previously. The third robot port is placed at the lateral border of the rectus in the right lower quadrant on the same line from the umbilicus to the ASIS. A 12-mm port is placed in the right lateral position for the assistant to pass suture into the abdomen and is used for retraction. An additional 5-mm assistant port is placed in the right upper quadrant, between the laparoscope port and right robot port. The suction irrigator is operated through this port by the assistant.
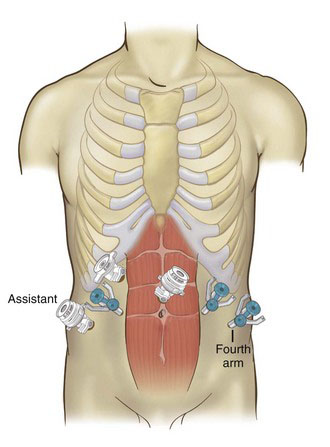
FIGURE 33-3 Trocar configuration during robot-assisted radical prostatectomy (teal blue = robotic 8-mm trocar).
Operative technique
1. Creation of the extraperitoneal space
2. Incision of the endopelvic fascia
3. Ligation of the dorsal venous complex
4. Division of the bladder neck
5. Dissection of the seminal vesicles and vas deferens
7. Nerve-sparing ligation of vascular pedicles
Creation of the Extraperitoneal Space
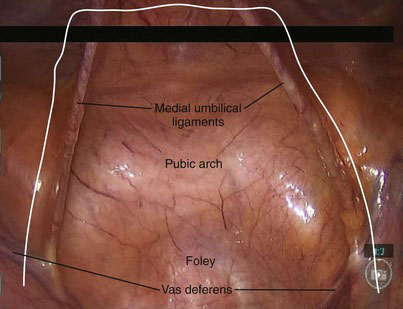
After gaining safe access to the abdomen and placing all trocars, the surgeon must mobilize the bladder to enter the extraperitoneal space (i.e., the space of Retzius, or retropubic space). The urachus and medial umbilical ligaments are divided high on the anterior abdominal wall using cautery or the ultrasonic scalpel. The peritoneum then is incised lateral to each umbilical ligament down posterior to the vas deferens (Fig. 33-4). The vas deferens is dissected and divided bilaterally. After the bladder has been mobilized from the anterior abdominal wall, the dome of the bladder is retracted cephalad to provide exposure to the pelvis. The assistant’s locking grasper retracts the bladder during LRP, whereas the fourth arm of the robot is used for this purpose during RARP.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree