Stress urinary incontinence (SUI), the involuntary leakage of urine associated with an increase in intraabdominal pressure (coughing, laughing, and sneezing), affects 12.8% to 46.0% of women. SUI is the most common type of urinary incontinence in women younger than 60 years and accounts for at least half of incontinence in all women. Retropubic and transobturator midurethral sling procedures are safe and effective treatments for stress urinary incontinence but have different complication profiles. History, examination, and additional testing may assist in choosing the correct sling type. Appropriate counseling and managing patient expectation are necessary to optimize patient satisfaction.
- •
Retropubic and transobturator midurethral sling procedures are safe and effective treatments for stress urinary incontinence but have different complication profiles.
- •
History, examination, and additional testing may assist in choosing the correct sling type.
- •
Appropriate counseling and managing patient expectation are necessary to optimize patient satisfaction.
- •
Women undergoing surgery for pelvic organ prolapse, both continent and incontinent, may benefit from concurrent midurethral sling placement.
Stress urinary incontinence
Stress urinary incontinence (SUI), the involuntary leakage of urine associated with an increase in intraabdominal pressure (coughing, laughing, and sneezing), affects 12.8% to 46.0% of women. SUI is the most common type of urinary incontinence in women younger than 60 years and accounts for at least half of incontinence in all women. Surgery for SUI represents one of the most common indications for surgery in women with more than 210,000 women undergoing surgery for SUI each year in the United States.
The midurethral sling
The tension-free vaginal tape (TVT) procedure was first introduced by Ulmsten and colleagues in 1996 and over the subsequent decade, gained worldwide popularity. This operation introduced 2 new concepts to the mechanism of cure for slings: placement at the midurethra and placement without tension or tension-free. The primary advantage of TVT over other surgical treatments for SUI available at the time, however, is that it could be performed in an outpatient. Often patients can void on the day of surgery and be discharged home without a catheter. Several randomized trials and numerous cohort studies suggest that the TVT procedure has similar cure rates to the Burch colposuspension with a quicker return to normal voiding and fewer postoperative complications. The success of the TVT has prompted the development of several similar minimally invasive midurethral slings with varying differences in sling material and surgical approach.
An innovation in the surgical management of SUI is the transobturator tape (TOT) ( Table 1 ), which was first described by Delorme in 2001. Similar to TVT, TOT is a minimally invasive midurethral sling that uses a synthetic tape; however, it is placed using a transobturator approach rather than a retropubic one ( Fig. 1 ). The impetus for the development of this technique was to reduce the risk of bladder perforation as well as eliminate the rare but life-threatening complications of bowel perforation and major vascular injury that have been reported with TVT. Published data are limited regarding the long-term efficacy of this new approach. A meta-analysis evaluating 11 randomized controlled trials comparing retropubic and transobturator approaches demonstrates similar effectiveness in overall and subjective outcomes. Objective outcomes were better with the retropubic approach.
| Special Case | Surgery | Rationale |
|---|---|---|
| Mixed urinary incontinence | TOT | TOT improves or does not exacerbate mixed urinary symptoms to the extent TVT may |
| ISD | TVT | Some but not all data indicate TVT is more effective for ISD |
| Non-mobile bladder neck | TVT | All sling procedures have lowered effectiveness when the bladder neck is immobile, consider periurethral bulking |
| With prolapse | TVT or TOT | Limited data support similar effectiveness for either approach |
| Occult SUI–leaks when prolapse reduced | TVT or TOT or staged | TOT has lower chance of creating new voiding symptoms; staging approach allows treatment of SUI if it develops |
| Recurrent SUI with history of sling complication or does not want mesh | N/A | May consider Burch, fascial sling or periurethral bulking |
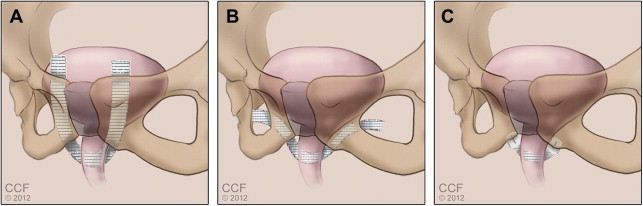
Most recently, the single-incision sling procedure for SUI, sometimes called mini-sling, was introduced with the goal of minimizing risk by avoiding the blind trocar passage through the retropubic or transobturator spaces associated with standard midurethral slings (see Fig. 1C ). As such, the single-incision sling procedure has the potential for fewer complications, less postoperative pain, and decreased anesthesia requirements compared with standard sling procedures. One such device, the TVT-SECUR (Ethicon Women’s Health and Urology, Somerville, NJ, USA), consists of an 8-cm polypropylene mesh with ends coated with an absorbable fleece material to provide fixation. This device can be placed using a retropubic or “U” approach or a transobturator-like “hammock” approach with clinical trials finding similar cure rates between the U and hammock approaches; however, quality of life and treatment satisfaction outcomes favor the U approach. A recent randomized controlled trial compared a single-incision sling (TVT-SECUR) to TVT, with the primary outcome of subjective cure of incontinence at 1 year. Results revealed similar subjective cure rates 1 year after surgery but greater postoperative incontinence severity with the single-incision sling compared with TVT. Other available single-incision slings are placed in a transobturatorlike approach using 1 of the fixation devices to anchor the sling into the obturator internus fascia.
Retropubic and transobturator midurethral sling procedures are safe and effective treatments for SUI but have different complication profiles. History, examination, and additional testing, such as urodynamics, can assist a surgeon in choosing the most appropriate sling for an individual patient ( Fig. 2 , Table 1 ).
The midurethral sling
The tension-free vaginal tape (TVT) procedure was first introduced by Ulmsten and colleagues in 1996 and over the subsequent decade, gained worldwide popularity. This operation introduced 2 new concepts to the mechanism of cure for slings: placement at the midurethra and placement without tension or tension-free. The primary advantage of TVT over other surgical treatments for SUI available at the time, however, is that it could be performed in an outpatient. Often patients can void on the day of surgery and be discharged home without a catheter. Several randomized trials and numerous cohort studies suggest that the TVT procedure has similar cure rates to the Burch colposuspension with a quicker return to normal voiding and fewer postoperative complications. The success of the TVT has prompted the development of several similar minimally invasive midurethral slings with varying differences in sling material and surgical approach.
An innovation in the surgical management of SUI is the transobturator tape (TOT) ( Table 1 ), which was first described by Delorme in 2001. Similar to TVT, TOT is a minimally invasive midurethral sling that uses a synthetic tape; however, it is placed using a transobturator approach rather than a retropubic one ( Fig. 1 ). The impetus for the development of this technique was to reduce the risk of bladder perforation as well as eliminate the rare but life-threatening complications of bowel perforation and major vascular injury that have been reported with TVT. Published data are limited regarding the long-term efficacy of this new approach. A meta-analysis evaluating 11 randomized controlled trials comparing retropubic and transobturator approaches demonstrates similar effectiveness in overall and subjective outcomes. Objective outcomes were better with the retropubic approach.
| Special Case | Surgery | Rationale |
|---|---|---|
| Mixed urinary incontinence | TOT | TOT improves or does not exacerbate mixed urinary symptoms to the extent TVT may |
| ISD | TVT | Some but not all data indicate TVT is more effective for ISD |
| Non-mobile bladder neck | TVT | All sling procedures have lowered effectiveness when the bladder neck is immobile, consider periurethral bulking |
| With prolapse | TVT or TOT | Limited data support similar effectiveness for either approach |
| Occult SUI–leaks when prolapse reduced | TVT or TOT or staged | TOT has lower chance of creating new voiding symptoms; staging approach allows treatment of SUI if it develops |
| Recurrent SUI with history of sling complication or does not want mesh | N/A | May consider Burch, fascial sling or periurethral bulking |
Most recently, the single-incision sling procedure for SUI, sometimes called mini-sling, was introduced with the goal of minimizing risk by avoiding the blind trocar passage through the retropubic or transobturator spaces associated with standard midurethral slings (see Fig. 1C ). As such, the single-incision sling procedure has the potential for fewer complications, less postoperative pain, and decreased anesthesia requirements compared with standard sling procedures. One such device, the TVT-SECUR (Ethicon Women’s Health and Urology, Somerville, NJ, USA), consists of an 8-cm polypropylene mesh with ends coated with an absorbable fleece material to provide fixation. This device can be placed using a retropubic or “U” approach or a transobturator-like “hammock” approach with clinical trials finding similar cure rates between the U and hammock approaches; however, quality of life and treatment satisfaction outcomes favor the U approach. A recent randomized controlled trial compared a single-incision sling (TVT-SECUR) to TVT, with the primary outcome of subjective cure of incontinence at 1 year. Results revealed similar subjective cure rates 1 year after surgery but greater postoperative incontinence severity with the single-incision sling compared with TVT. Other available single-incision slings are placed in a transobturatorlike approach using 1 of the fixation devices to anchor the sling into the obturator internus fascia.
Retropubic and transobturator midurethral sling procedures are safe and effective treatments for SUI but have different complication profiles. History, examination, and additional testing, such as urodynamics, can assist a surgeon in choosing the most appropriate sling for an individual patient ( Fig. 2 , Table 1 ).
Indications for surgery
Surgery is indicated for the treatment of SUI when conservative treatments have failed to satisfactorily relieve the symptoms, and the patient wishes further treatment in an effort to achieve continence. Although most experts agree that surgery should be delayed until childbearing is complete, the desire for future childbearing should not be considered an absolute contraindication. Before surgery, stress incontinence should be objectively documented with direct visualization of urine loss from the urethra with stress. See Box 1 for the recommended minimum evaluation for women complaining of SUI. Not all patients with urinary incontinence require urodynamic testing before surgery, and emerging data question the utility of urodynamics. However, urodynamics should be considered before surgery if the diagnosis is unclear or the patient is at high-risk for treatment failure or complications ( Box 2 ). Traditional teaching requires that urethral hypermobility be demonstrated with Q-tip testing or some similar method. However, the authors do not consider this an absolute requirement.
- •
Comprehensive history
- •
Physical examination
- •
Urinalysis
- •
Measurement of postvoid residual volume
- •
Direct visualization of urine loss from the urethra during cough or valsalva
- •
Urethral hypermobility should be evaluated with Q-tip testing or some similar method
- •
Unclear history
- •
Advanced age
- •
History of previous continence surgery
- •
Symptoms suggestive of detrusor overactivity or voiding dysfunction
- •
Abnormal sacral neurologic examination
- •
Increased postvoid residual volume
Factors that may negatively influence the results of SUI surgery include advancing age, obesity, history of previous incontinence surgery, nonmobile urethra, and preoperative detrusor overactivity ( Box 3 ). However, the evidence supporting these negative predictors is generally weak. As such, these factors should not be considered contraindications to continence surgery, but instead be used for patient counseling. Contraindications to SUI surgery include the presence of pure detrusor overactivity and an atonic bladder or a neurogenic bladder ( Box 4 ). Also, patients who are otherwise at high risk for postoperative urinary retention who are unable or unwilling to perform self-catheterization may not be good candidates for SUI surgery.





