The midurethral sling (MUS) is now the most commonly performed surgical treatment for stress urinary incontinence (SUI), and is considered the gold standard for patients with genuine SUI. This article examines the use of the MUS to treat all forms of SUI, with an emphasis on the nonindex patient (ie, intrinsic sphincter deficiency, lack of urethral hypermobility, mixed incontinence, failed MUS, concomitant prolapse, obesity, and elderly). The efficacy and safety of the MUS to treat SUI is assessed in these specific populations. Based on the available evidence, the discussion attempts to identify populations in whom MUS may not be appropriate.
- •
The midurethral sling (MUS) is the gold standard for stress urinary incontinence (SUI) in the index patient, with equivalent outcomes and minimal adverse events in comparison with traditional SUI procedures.
- •
With appropriate patient counseling, the MUS can be considered first-line therapy for more complicated situations as well.
- •
Complicated situations include intrinsic sphincter deficiency, lack of urethral hypermobility, mixed urinary incontinence, prior failed MUS, concomitant pelvic organ prolapse repair, and obese and elderly populations.
- •
The pubovaginal sling is still preferred for patients in whom synthetic mesh is contraindicated, or in neurogenic SUI whereby obstruction is desired.
In July 2011, the Food and Drug Administration (FDA) issued a statement directed at transvaginal “surgical mesh implanted to repair pelvic organ prolapse (POP) and/or stress urinary incontinence (SUI),” stating that “serious complications associated with surgical mesh for transvaginal repair of POP are not rare,” and its use “has not been shown to improve clinical benefit over traditional non-mesh repair.” In particular, the FDA identified vaginal mesh erosion (also called exposure, extrusion or protrusion) and contraction as significant complications, with a higher incidence than that reported in its statement in 2008. On this basis, it recommended consideration of a change in risk classification for transvaginal mesh devices from class II to class III, which could require manufacturers to provide extensive preclinical testing data demonstrating efficacy and safety. The FDA also recommended further clinical studies addressing the risks and benefits of mesh in the treatment of POP and SUI, and expanded postmarket monitoring of mesh-device performance.
The FDA convened a panel to address their statement in September 2011, including presentations from various professional societies including the American Urological Association (AUA), Society for Female Urology and Urodynamics, and American Urogynecologic Society, among others. The AUA and other groups supported the FDA’s motion for further clinical studies, rigorous patient consent, appropriate surgeon education and credentialing, and expanded postmarket surveillance of mesh devices. However, the AUA strongly reinforced the need to differentiate between the use of mesh to treat POP versus SUI, citing the existence of extensive data supporting the efficacy of synthetic mesh at the midurethra to treat SUI with minimal morbidity compared with conventional nonmesh procedures. The AUA released a position statement in November 2011 reiterating these points. The FDA is currently considering the panel’s recommendations, and a decision is pending.
Introduction
The midurethral sling (MUS) is now the most commonly performed surgical treatment for stress urinary incontinence (SUI). It is considered the gold standard for patients with genuine SUI. Encouraged by the excellent outcomes and low morbidity in these index patients, clinicians have extended the use of the MUS to treat SUI in more complex situations, such as recurrent SUI, mixed urinary incontinence (MUI), and SUI in the elderly or obese. However, whether an MUS can be recommended for all cases of SUI remains controversial.
This article examines the use of the MUS to treat all forms of SUI, with an emphasis on the nonindex patient. This category includes complex SUI or other circumstances that clinicians commonly encounter. Starting with a brief history of slings, the outcomes of retropubic and transobturator slings in the uncomplicated patient are reviewed. The efficacy and safety of the MUS to treat SUI is then assessed in the following special populations: intrinsic sphincter deficiency (ISD), lack of urethral hypermobility, MUI, recurrent SUI after failed MUS placement, concomitant pelvic organ prolapse (POP) repair, and obese and elderly patients. Based on the available evidence, the discussion herein attempts to identify the populations in whom MUS may not be appropriate in comparison with those who may expect good to excellent outcomes.
History
In 1997, the AUA Female Stress Incontinence Clinical Guidelines Panel concluded that the retropubic suspensions and pubovaginal sling (PVS) were the most effective treatments for SUI, reflecting the widespread sentiment that these procedures represented the gold standard at that time. Only 2 years earlier, Ulmsten and Petros first described the tension-free vaginal tape (TVT), a retropubic midurethral synthetic sling that was considerably less invasive with high short-term success rates. Because of the relative ease of performance and very good initial results, it quickly became one of the most commonly performed procedures and inspired the development of various other MUSs. Most notably, in 2001 Delorme introduced the transobturator sling placed through the obturator foramina, which was intended to avoid the retropubic space and its potential major complications.
The first validation of the MUS as a first-line procedure for SUI came from Ward and Hilton, who performed a multicenter randomized controlled trial (RCT) showing no significant differences in efficacy and safety of the TVT compared with the then gold-standard Burch colposuspension. Several RCTs have confirmed their findings, culminating in the most recent meta-analysis by Novara and colleagues, which found that the MUS is more effective than the Burch colposuspension and equally as effective as the PVS in achieving objective cure of SUI. Thus, the MUS has effectively been established as the new gold standard for surgical treatment of SUI.
There are currently even less invasive developments of the MUS, known as minislings or single-incision slings, which are placed through a vaginal incision without any exit incisions. These newer slings are currently under study and have not yet been proved to be equivalent or less morbid than traditional MUS, and as such are not addressed in this review.
Anatomic approaches
The Integral theory of Petros and Ulmsten and the Hammock hypothesis of Delancey led to insights on the importance of urethral configuration and its supporting structures in the efficient transmission of closure pressure in maintaining continence, ultimately focusing at the midurethra. Based on the Integral theory, the original TVT aimed to reinforce the weakened pubourethral ligaments, restoring compression at the midurethra and resulting in continence. Subsequent ultrasound studies have confirmed this compressive effect at the level of the midurethra, and have also demonstrated a dynamic kinking effect by the MUS based on providing stability at the posterior midurethra.
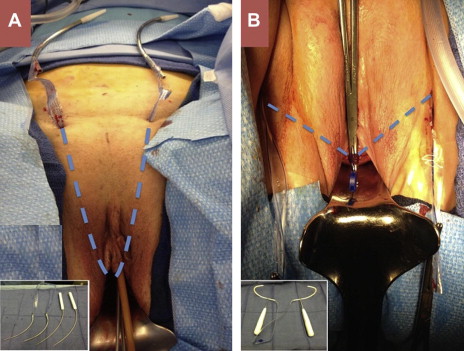
There are 2 main approaches in placing a sling at the level of the midurethra. The retropubic route was used by the original TVT, passing trocars from a midurethral incision through the endopelvic fascia and retropubic space and exiting at the suprapubic area (see Fig. 1 A for an example of this approach). The transobturator route was subsequently introduced, passing a helical trocar from the groin past the adductor muscle of the leg through the obturator foramen, and exiting the vaginal incision (see Fig. 1 B for an example of this approach). Numerous technical variations in the direction of trocar passage have been developed for both approaches ( Table 1 ).
| Name | Type | Manufacturer |
|---|---|---|
| TVT | Retropubic bottom-top | Ethicon |
| Advantage | Retropubic bottom-top | Boston Scientific |
| SPARC | Retropubic top-bottom | AMS |
| Lynx | Retropubic top-bottom | Boston Scientific |
| MONARC | Transobturator outside-in | AMS |
| ObTryx | Transobturator outside-in | Boston Scientific |
| Aris | Transobturator outside-in | Coloplast |
| TVT-O | Transobturator inside-out | Ethicon |
History
In 1997, the AUA Female Stress Incontinence Clinical Guidelines Panel concluded that the retropubic suspensions and pubovaginal sling (PVS) were the most effective treatments for SUI, reflecting the widespread sentiment that these procedures represented the gold standard at that time. Only 2 years earlier, Ulmsten and Petros first described the tension-free vaginal tape (TVT), a retropubic midurethral synthetic sling that was considerably less invasive with high short-term success rates. Because of the relative ease of performance and very good initial results, it quickly became one of the most commonly performed procedures and inspired the development of various other MUSs. Most notably, in 2001 Delorme introduced the transobturator sling placed through the obturator foramina, which was intended to avoid the retropubic space and its potential major complications.
The first validation of the MUS as a first-line procedure for SUI came from Ward and Hilton, who performed a multicenter randomized controlled trial (RCT) showing no significant differences in efficacy and safety of the TVT compared with the then gold-standard Burch colposuspension. Several RCTs have confirmed their findings, culminating in the most recent meta-analysis by Novara and colleagues, which found that the MUS is more effective than the Burch colposuspension and equally as effective as the PVS in achieving objective cure of SUI. Thus, the MUS has effectively been established as the new gold standard for surgical treatment of SUI.
There are currently even less invasive developments of the MUS, known as minislings or single-incision slings, which are placed through a vaginal incision without any exit incisions. These newer slings are currently under study and have not yet been proved to be equivalent or less morbid than traditional MUS, and as such are not addressed in this review.
Anatomic approaches
The Integral theory of Petros and Ulmsten and the Hammock hypothesis of Delancey led to insights on the importance of urethral configuration and its supporting structures in the efficient transmission of closure pressure in maintaining continence, ultimately focusing at the midurethra. Based on the Integral theory, the original TVT aimed to reinforce the weakened pubourethral ligaments, restoring compression at the midurethra and resulting in continence. Subsequent ultrasound studies have confirmed this compressive effect at the level of the midurethra, and have also demonstrated a dynamic kinking effect by the MUS based on providing stability at the posterior midurethra.
There are 2 main approaches in placing a sling at the level of the midurethra. The retropubic route was used by the original TVT, passing trocars from a midurethral incision through the endopelvic fascia and retropubic space and exiting at the suprapubic area (see Fig. 1 A for an example of this approach). The transobturator route was subsequently introduced, passing a helical trocar from the groin past the adductor muscle of the leg through the obturator foramen, and exiting the vaginal incision (see Fig. 1 B for an example of this approach). Numerous technical variations in the direction of trocar passage have been developed for both approaches ( Table 1 ).
| Name | Type | Manufacturer |
|---|---|---|
| TVT | Retropubic bottom-top | Ethicon |
| Advantage | Retropubic bottom-top | Boston Scientific |
| SPARC | Retropubic top-bottom | AMS |
| Lynx | Retropubic top-bottom | Boston Scientific |
| MONARC | Transobturator outside-in | AMS |
| ObTryx | Transobturator outside-in | Boston Scientific |
| Aris | Transobturator outside-in | Coloplast |
| TVT-O | Transobturator inside-out | Ethicon |
Results of MUS in the general population
There is a vast body of literature reporting on MUS, from which several recent high-quality reviews have provided support for the use of both retropubic and transobturator slings to treat SUI. Most of the early RCTs of MUS, including comparator RCTs to colposuspension and PVS, were performed with a favorable population (the index patient) that excluded conditions such as concomitant prolapse repair, detrusor overactivity (DO), or prior surgery. In brief, in comparing the retropubic and transobturator approaches, the following conclusions can be made based on the Cochrane meta-analysis by Ogah and colleagues regarding the efficacy and complications of MUS in this population:
Efficacy. For retropubic versus transobturator approach: retropubic slings have a slightly higher objective cure rate (88% vs 84%), but there is no difference in subjective cure rate (83% for both groups in the Cochrane meta-analysis).
Complications. Transobturator slings have a higher incidence of transient groin pain (12%), but retropubic slings have a higher risk of bladder perforation (5.5% vs 0.3%) and postoperative voiding dysfunction (7% vs 4%). The recent review by Novara and colleagues confirmed all of these findings, and also found that retropubic slings have a higher rate of hematoma (odds ratio [OR] 2.62, 95% confidence interval [CI] 1.75–3.57) and vaginal perforation (OR 2.62, 95% CI 1.35–5.08), as well as storage lower urinary tract symptoms (OR 1.35, 95% CI 1.05–1.72).
Based on these data, the literature supports the use of either retropubic or transobturator slings to effectively and safely treat the index patient with SUI, with a slight advantage to the transobturator approach with regard to perioperative and long-term complications. What follows is a discussion of the use of MUS in the treatment of more complex SUI, with the intent of determining whether MUS is appropriate for all forms of SUI.
Intrinsic sphincter deficiency and urethral hypermobility
Patients with SUI have traditionally been classified in terms of 2 parameters: defects in the anatomic support of the urethra (urethral hypermobility) versus incompetence of the sphincter itself, commonly referred to as ISD. Current thinking has evolved away from this dichotomy with the understanding that most patients lie on a spectrum with some degree of both hypermobility and ISD. In ISD, the poorly functioning sphincter may be due to aging, previous surgery, radiation therapy, or neurologic insult.
Although there is no standardized definition, ISD has been defined in the literature based on the urodynamic findings of Valsalva leak-point pressure (VLPP) of less than 60 cm H 2 O or maximum urethral closure pressure (MUCP) of less than 20 cm H 2 O. Women with ISD have been reported to have more severe incontinence with a higher risk of treatment failure, and historically the PVS was recommended in such cases, with cure rates of 80% to 85%. Though excluded from most series initially, there are now several studies on both retropubic and transobturator MUS in this population.
Rezapour and colleagues first reported their favorable and durable results using TVT in 49 women with ISD (defined as MUCP <20 cm H 2 O, not VLPP) with a cure rate of 74% and significant improvement in 12%, which approaches their success rates in the general population. Of note, only 8 patients did not have urethral hypermobility (as defined by Q-tip test >30°), and of the 7 failures, 5 had fixed urethras. Although the numbers were small, the investigators suggested that lack of hypermobility may be a risk factor for failure.
Subsequently several studies have compared retropubic to transobturator approaches in patients with ISD (defined by VLPP <60 cm H 2 O or MUCP <20 cm H 2 O). Jeon and colleagues retrospectively compared TVT, transobturator tape (TOT), and the PVS in women with ISD at 2 years’ follow-up. Patients with TVT had cure rate of 86.9%, similar to the 87.3% seen with PVS, in contrast to the TOT group, which had only 34.9% cure ( P <.0001). At 31 months, Gungorduk and colleagues found cure rates of 78.3% using TVT versus 52.5% using TOT, and reported that TOT was 5 times more likely to fail than TVT in women with ISD, similar to previously reported short-term results of Miller and colleagues. In the only prospective, randomized study addressing this issue, Schierlitz and colleagues randomized 164 women with ISD to TVT or TOT, with the primary outcome of urodynamic SUI at 6 months. Twenty-one percent of the TVT group had SUI on urodynamics versus 45% in the TOT group ( P = .004). Moreover, 13% of women in the TOT group requested a repeat sling, compared with none in the TVT group.
The literature suggests that retropubic slings work well for patients with ISD but obturator slings may not work as well. By contrast, a retrospective study by Rapp and colleagues found no difference between retropubic and transobturator slings in women with ISD with success rates of 76% and 77%, respectively. Costantini and colleagues also reported no difference between TVT and TOT in women with ISD using a subset analysis of their RCT, although it should be emphasized that all of their patients had hypermobility ranging from 43° to 90° by Q-tip test. These investigators found no difference in outcome between 45 TVT patients and 50 TOT patients at 35 months (68% vs 76%, respectively). Although this was a post hoc analysis that was underpowered to detect a difference, the data do suggest that if ISD patients have concurrent hypermobility the results may be different, particularly with the transobturator approach.
A recent study by Haliloglu and colleagues examined the impact of ISD and urethral hypermobility in 65 TOT patients by dividing them into 3 groups: ISD with hypermobility (n = 18), ISD with fixed urethra (n = 16), and hypermobility without ISD (n = 31). At 24 months the 2 groups with hypermobility had similar cure rates, with and without ISD (87.5% and 96.4%, respectively). However, those with no hypermobility had a significantly lower cure rate, at 66.7%. Minaglia and colleagues studied urethral hypermobility independent of ISD in 107 women undergoing TOT, and found that women with urethral mobility of less than 45° were 4 times more likely to have persistent SUI than women with urethral mobility greater than 45° (29.4% vs 6.9%, respectively, P = .005). Hypermobility was also a predictive factor in patients undergoing TVT in a series reported by Fritel and colleagues, with success rates of 92% with Q-tip test greater than 30° versus 70% for Q-tip test less than 30°. ISD defined as MUCP less than 20 cm H 2 O had no impact on success rate.
Taken together, retropubic and transobturator MUS procedures appear to be effective in treating patients with ISD and hypermobility. The literature suggests that a less mobile urethra is a risk factor for transobturator sling failure, and in these cases the retropubic approach may be favored.
Mixed urinary incontinence
MUI refers to the complaint of involuntary leakage associated with urgency and also with exertion, effort, sneezing, or coughing. Patients with MUI may be difficult to treat, as postoperative incontinence may occur secondary to both recurrent SUI and persistent or de novo urge urinary incontinence (UUI). Moreover, women with MUI who undergo surgery may expect resolution of UUI as well. There are now data and expert consensus to support the use of stress incontinence procedures in patients with MUI and a significant SUI component. Not surprisingly, both retropubic and transobturator MUS has shown to have excellent cure rates for the stress component, reported to range from 85% to 97% in a recent review by Jain and colleagues. Recent research has analyzed the efficacy of MUS in treating the urge component, as well as which factors predict better or worse outcomes.
Duckett and Tamilselvi reported on a series of 46 patients with SUI and DO confirmed on urodynamics. Six months after TVT, 63% reported subjective resolution of urge symptoms, and 47% had objective resolution of DO on postoperative urodynamics. Paick and colleagues reported even higher cure rates in women with MUI undergoing TVT, SPARC, and TOT at 11 months, with resolution of both SUI and UUI in 81.9%, 77.3%, and 78%, respectively. However, they included all patients complaining of UUI with or without DO, and in fact DO was associated with a 3.4-fold risk of treatment failure in this series. Of note, the TOT group had significantly less severe preoperative UUI than both retropubic groups.
In contrast to these promising short-term results, studies with a longer follow-up have demonstrated less encouraging outcomes. Kulseng-Hanssen and colleagues reported on a series of 1113 patients with MUI at 38 months after TVT and found a subjective cure rate of 53.8%. When stratified into patients with predominantly UUI, the subjective cure rate was only 38.4%; however, patients’ satisfaction was still 60%. Holmgren and colleagues reported on 112 women with MUI treated with TVT, but with longer follow-up of up to 8 years. In a cross-sectional analysis, 61 women followed for 2 to 3 years had 60% self-reported cure of MUI, but of the 30 women followed for 5 to 8 years only 30% to 40% reported cure. Conversely, Lee and colleagues reported 6-year outcomes in 34 women with MUI, and reported subjective cure rates by validated questionnaire to be similar to those for 107 women with pure SUI (79.4% vs 84.1%).
There are several studies comparing efficacy of retropubic and transobturator slings for the treatment of women with MUI. Gamble and colleagues reported on 305 women with SUI and DO undergoing TOT, TVT, SPARC, or bladder-neck slings. The primary outcome was persistent DO at 3 months. Resolution of DO differed significantly between the groups, with the best results after TOT (47%), followed by retropubic slings (36% after TVT, 37% after SPARC) and bladder-neck slings (14%) ( P <.001). Subjective cure of UUI was seen in 44% of the whole group, and although cure rates for each sling type were not provided, they reported that sling type predicted persistent UUI. Compared with TOT patients, patients with retropubic and bladder-neck slings were 2 times and 4 times more likely to report persistent UUI, respectively. By contrast, a similar study by Botros and colleagues found no difference in resolution of DO at 3 months in retropubic versus transobturator slings. In a large observational cohort, Lee and colleagues studied 514 women with MUI and 754 women with SUI and urge symptoms (but no UUI) who were treated with retropubic or transobturator slings. At a mean follow-up of 50 months, there was resolution of UUI in 67.7% and urge symptoms in 59.7%. The transobturator approach was a significant predictor for resolution of urgency although it did not affect cure of UUI. Preoperative DO was once again a risk factor for persistent UUI and urgency.
It can be concluded from the available literature that for patients with MUI, MUS effectively treats the SUI and can also cure UUI in at least 50% of the patients in the short term; however, the UUI seems to recur over time. The transobturator approach appears to provide the best control of urgency and DO. However, patients must be counseled extensively because the risk of persistent urge symptoms remains high, particularly in those who have preoperative DO.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




