• Excretion of ammonium 
■ Thus, metabolic acidosis can result from failure to reclaim bicarbonate in the proximal tubule or failure to secrete acid in the distal tubule.
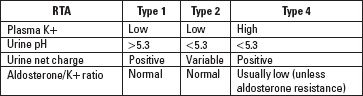
■ Hypokalemic distal RTA (type 1) is due to impaired secretion of H+ from the alpha-intercalated cells in the CD. Increased secretion of K+ also occurs, resulting in hypokalemic hyperchloremic acidosis. The most common causes are hereditary, autoimmune disease, tubulointerstitial disease, and dysproteinemias. Urine pH is increased (>5.3) despite systemic acidosis. There is decreased  excretion, resulting in decreased excretion of the accompanying Cl− anion; thus, urinary Na+ + K+ > Cl− (this is referred to as positive urine “net charge” or urine anion gap [defined as UNa+ + UK+ − UCl−]).
excretion, resulting in decreased excretion of the accompanying Cl− anion; thus, urinary Na+ + K+ > Cl− (this is referred to as positive urine “net charge” or urine anion gap [defined as UNa+ + UK+ − UCl−]).
■ Proximal RTA (type 2) is due to failure to reabsorb filtered bicarbonate. It is often accompanied by other features of Fanconi syndrome. The most common causes are dysproteinemias and drugs (carbonic anhydrase inhibitors). Urine pH is less than 5.3. Calculation of urine net charge or anion gap is not useful as it has been shown to be variable in different studies.
■ Hyperkalemic distal RTA (type 4). This is usually due to hypoaldosteronism or aldosterone resistance in the setting of CKD. The resultant hyperkalemia leads to decreased  excretion (due to inhibition of ammonia formation). Most common causes are diabetes (hyporeninemic hypoaldosteronism thought to be primarily due to glycation of prorenin with impaired activation to renin), drugs (renin–angiotensin–aldosterone [RAAS] axis inhibitors, aldosterone synthesis inhibitors such as heparin, and inhibitors of tubular K+ secretion such as trimethoprim and calcineurin inhibitors). NSAIDs inhibit the RAAS as well as tubular K+ secretion. Urine pH is less than 5.3. Urinary Na+ + K+ > Cl− (positive urine “net charge”).
excretion (due to inhibition of ammonia formation). Most common causes are diabetes (hyporeninemic hypoaldosteronism thought to be primarily due to glycation of prorenin with impaired activation to renin), drugs (renin–angiotensin–aldosterone [RAAS] axis inhibitors, aldosterone synthesis inhibitors such as heparin, and inhibitors of tubular K+ secretion such as trimethoprim and calcineurin inhibitors). NSAIDs inhibit the RAAS as well as tubular K+ secretion. Urine pH is less than 5.3. Urinary Na+ + K+ > Cl− (positive urine “net charge”).
Summary of Major Laboratory Findings in RTA
Q1: A 22-year-old male medical student weighing 72 kg undergoes blood chemistry measurements as part of a class project to study renal physiology. His plasma creatinine is 1.0 mg per dL (88.4 mcmol/L). Although his plasma creatinine is in the normal range, he is concerned that he may have kidney disease, and so he does a urinalysis, which is normal, and collects a 24-hour urine for measurement of CCr. His 24-hour urine creatinine excretion is 1,440 mg (12.7 mmol) in a volume of 1,440 mL. What is his CCr?
A1: The first consideration is whether the 24-hour urine was completely collected. The student relates that he voided all the urine in his bladder at 7:00 AM into the toilet and then collected all his urine until 7:00 AM the following day, which is the correct procedure. The amount of creatinine in the urine is 20 mg per kg (177 mcmol/kg). Creatinine excretion depends on muscle mass, and normal ranges are 14 to 26 mg per kg (124–230 mcmol/kg) for men and 11 to 20 mg per kg (97–177 mcmol/kg) for women. Thus, this appears to be a complete collection.
Now we wish to determine the CCr. As CCr = [(urine creatinine concentration) × (urine flow rate)]/plasma creatinine concentration, and creatinine excretion rate = urine creatinine concentration × urine flow rate, CCr = creatinine excretion rate/plasma creatinine. The only problem is that creatinine excretion rate is in mg (or mmol)/24 hours and plasma creatinine is in mg/dL (or mmol/L), so we need a correction factor to arrive at a CCr in mL/min. In the above example, this can be determined as follows:
CCr = creatinine excretion rate (1,440 mg/24 h)/plasma creatinine (1.0 mg/dL) = 1,440 dL/24 h.
In order to convert to mL/min, one needs to do the following:
1,440 dL/24 h × 100 mL/dL × 24 h/1,440 min = 100 mL/min. Since 100/1,440 = 0.07, a quick way to calculate this is:
CCr (mL/min) = [creatinine excretion rate (mg/24 h)/plasma creatinine (mg/dL)] × 0.07
Another option is to convert mg/24 hour to mg/min and plasma creatinine to mg/mL (as we did in the example at the beginning of the chapter), which will give you (1.0 mg/min)/(0.01 mg/mL) = 100 mL/min. However, this method, although good for illustration with nice numbers as in this case, does not work out as well in practice as the “0.07 correction factor” method.
Why not calculate CCr the more “usual” way taught in medical school? That is,
CCr = (urine creatinine concentration × urine flow rate)/(plasma creatinine concentration × 1440)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


