The role of varicocelectomy in management of male subfertility
Background
Varicocele is present in approximately 40% of men presenting with infertility [1]. Although varicocele repair is widely used in the management of male-factor infertility, the effectiveness of varicocelectomy has been intensely debated, and there is still no consensus on the topic.
Existing literature is conflicting, and very few sufficiently large and adequately controlled prospective trials are available evaluating the efficacy of varicocelectomy in improving pregnancy outcomes. Two published meta-analyses evaluating prospective randomized trials came to the same conclusion that varicocele repairs do not improve subfertility [2,3]. A recently updated Cochrane review recommended against varicocele repair for unexplained infertility [4]. However, these meta-analyses have been criticized for methodological flaws which may have biased their results [5]. Consequently, they have not resolved the issues surrounding varicocelectomy and subfertility.
The development of assisted reproductive techniques (ART) has led to increased use of intracytoplasmic sperm injection (ICSI) for all causes of male infertility including varicoceles. However, these techniques have safety issues, deprive patients of the satisfaction of natural conception, and are less cost-effective [6].
Recent guidelines from the Best Practice Policy Committee of the American Urological Association (AUA) and the American Society for Reproductive Medicine (ASRM) have recommended varicocele repair for infertile men with a clinically palpable varicocele and at least one or more abnormal semen parameters with female partner having either normal or potentially treatable fertility [7].
Rationale for the use of varicocelectomy in management of male subfertility
The exact mechanism by which varicocelectomy improves fertility in affected men remains unknown. Oxidative stress and DNA damage to sperm, which are well-documented components of varicocele pathophysiology, have shown improvement after varicocele repair. Hurtado de Catalfo and colleagues have demonstrated elevated levels of thiobarbituric acid reactive substances which are markers of oxidative stress in both seminal and peripheral plasma of varicocele patients which returned to normal 1 month post varicocelectomy. Other markers of oxidative stress were also decreased and the total antioxidant capacity was increased 6 months after varicocelectomy in their study [8]. Confirming the increased antioxidant capacity after varicocele repair, a more recent study also found a significant decrease in the levels of 8-hydroxy-2-deoxy-guanosine (8-OHdG), another marker of oxidative stress in all postvaricocele repair patients. In this study, investigators also demonstrated a significant decline in the incidence of 4977 bp deletion in mitochondrial DNA, a marker of oxidant-mediated DNA damage after varicocele repair [9]. Shiraishi & Naito showed that elevated preoperative 4-hydroxy-2-nonenal (4-HNE) modified protein levels in the testis could predict a response to varicocele repair [10]. These landmark studies have suggested that varicocele repair decreases the levels of oxidative stress as a mechanism for improving fertility.
Literature search
We conducted new meta-analyses to assess the effect of varicocelectomy on pregnancy outcomes and semen parameters [11,12]. In these analyses, we included both randomized controlled trials and observational studies. Although critics may object to inclusion of observational studies in a meta-analysis, we adhered to the principles of the Potsdam guidelines laid down by a group of 20 scientists for the conduct and interpretation of meta-analyses [13].
Studies were identified by performing an extensive search using BIOSIS, EMBASE, and Medline (from 1985 to the present) with the help of a professional librarian as well as by hand-searching review articles and cross-references. The following keywords were used to search the databases: “varicocelectomy,” “microsurgery,” “high ligation,” “infertility,” “semen parameters,” and “pregnancy or outcome.” No exclusions were made based on language. Studies were excluded if subclinical varicocele only or subclinical varicocele combined with clinical varicocele were examined or if the effect of treatment was examined only in an adolescent population.
Types of participants
Infertile males diagnosed with unilateral or bilateral varicoceles with abnormal semen parameters. The control groups were composed of infertile males with varicocele who declined to undergo surgical repair of varicocele, were randomized to no/medical treatment or randomized to receive treatment after the follow-up period.
Types of intervention
Surgical ligation (high ligation, inguinal or microsurgery).
Types of outcome measures
- Effect of varicocelectomy on semen parameters – change in semen parameters (count, motility and morphology) after surgery using before-and-after repeated measures studies. These studies had semen data from the same individual, before and after varicocelectomy.
- Effect of varicocelectomy on pregnancy outcome – proportion of couples achieving spontaneous pregnancy during follow-up of up to 24 months using observational and randomized controlled trials.
Effect of varicocelectomy on semen parameters
Blinding and scoring.
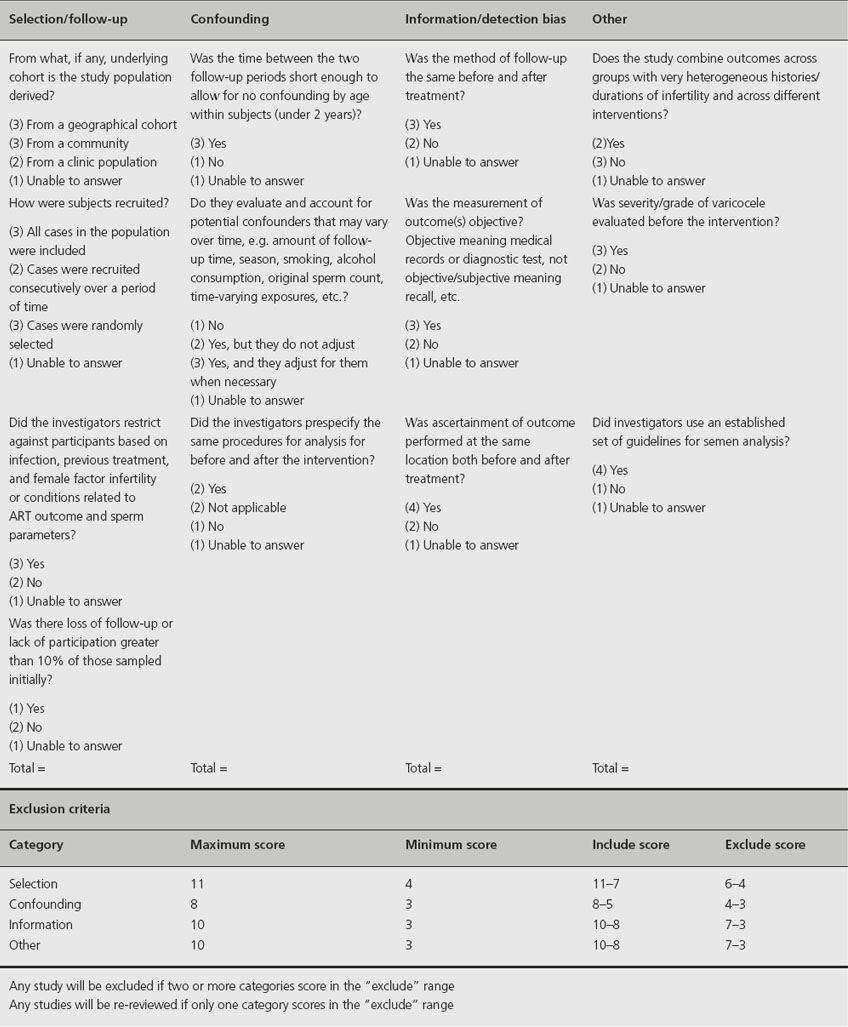
All articles and reviewers were blinded during the evaluation period. Two evaluators blinded to the concluding results, authors, journal, and year of the articles evaluated each study on its methodological merits. Articles with both pre- and postoperative repeated measures of semen parameters were evaluated for methodological qual-ity by our new scoring system (Table 16.1). The questions and scores were developed to evaluate four categories of bias: selection or follow-up bias, confounding bias, information or detection bias, and other sources of bias such as misclassification. If the points for more than one category of bias totaled to below an acceptable range, the study was automatically excluded from the final analysis. If the points for only one category totaled below the acceptable range, the study was re-examined to determine whether the overall study was likely to be biased and, if not, whether it could be included in the meta-analysis. If the follow-up time was more than 2 years after the surgery or with no follow-up within this time period or if the study did not account for time-varying confounders, then it was likely that the study would be excluded. Two reviewers scored each study independently, and the final decision on whether or not a study was to be included was determined by a discussion between the two reviewers.
Table 16.1 Scoring sheet used to evaluate studies
Data extraction.
Data were extracted by one of the investigators on a preformatted data extraction sheet. The outcomes of interest for continuous variables such as concentration, motility and morphology data were extracted, and a weighted mean was calculated. Population information (i.e. primary versus secondary infertility) and study characteristics such as the specific intervention (high ligation, microsurgery, and laparoscopy) were listed.
Data analysis.
The data were then entered in the RevMan software (version 4.2.8) developed by the Cochrane Collaboration for the purpose of meta-analysis (www.cochrane.org). The semen data were segregated according to the type of surgical procedure used on these patients. Studies were included that had at least three semen analyses per patient. Since sequential semen data often demonstrate variability, a random effects model was used to adjust for the heterogeneity. A p value < 0.05 was used as a cut-off point for significance testing in all statistical tests.
Effect of varicocelectomy on pregnancy outcome
To examine the effect of varicocelectomy on “spontaneous or natural” pregnancy outcome, cohorts were studied within a 2-year follow-up, after a varicocelectomy was performed on one cohort and no/medical treatment or no surgical treatment on another. Studies were retrieved in the same manner as described above for semen characteristics. They were then graded using a scoring sheet that was specifically intended to examine the research question. The development of the scoring criteria was similar to that described above with the same considerations of bias, but other questions were developed for cohort studies rather than pre/post repeated measures studies. Studies were excluded if they had men with subclinical varicoceles. Patients who had undergone ART were not included in the analysis. Studies that used embolization or sclerosis techniques for varicocele corrections were also excluded.
Extraction of data was performed without a data extraction sheet because there was only one outcome of interest. Pregnancy data were recorded for the 24-month interval after surgery and the overall odds were calculated. The data were verified by a second investigator, and analysis of the pregnancy data was performed by both random and fixed effects models.
Clinical question 16.1
What is the effect of varicocelectomy on semen parameters?
Trials included
A total of 136 studies were identified, of which only17 were included in the meta-analysis that pertained to semen parameters [14–30].
Outcomes
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








