Magnetic Resonance Urography
Magnetic resonance (MR) urography refers to MR imaging (MRI) of the urinary collecting systems in a way that provides information roughly analogous to conventional intravenous urography (IVU). Magnetic resonance imaging is well suited to evaluation of the urinary collecting systems for several reasons. First, the collecting systems are fluid-filled structures that can be imaged using techniques described for magnetic resonance cholangiopancreatography (MRCP). Second, the multiplanar capability of MRI allows optimization of scan planes for evaluation of the ureters and bladder. Third, the extracellular gadolinium chelates are excreted by glomerular filtration. In addition to providing excellent anatomic depiction of the kidneys and renal collecting systems, gadolinium chelates allow functional studies of the collecting systems to be performed without aggravating or inducing renal insufficiency. Despite these theoretical advantages, MR urography is rarely performed as a standalone procedure, because conventional IVU, computed tomography (CT), or ultrasound suffices for diagnosis of the majority of urologic abnormalities. However, MR urography remains a useful adjunct technique when combined with renal parenchymal imaging, particularly in patients with compromised renal function.
Technique
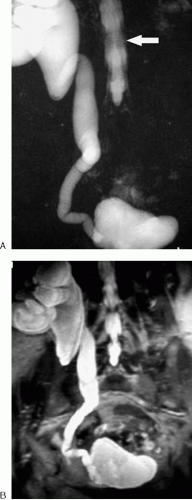
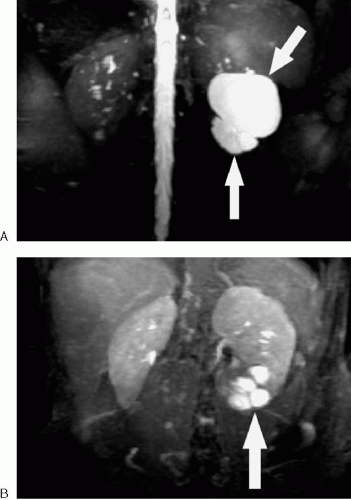
The simplest method of performing MR urography involves the use of long echo train, heavily T2-weighted sequences identical to those employed for MRCP. This method is often referred to as static MR urography, and long echo train T2-weighted sequences are sometimes referred to as RARE (rapid acquisition with relaxation enhancement) sequences. The use of a relatively long effective echo time (TE) (>140 msec) results in greater conspicuity of fluid-containing structures. The use of fat suppression further increases conspicuity of the collecting systems by eliminating signal from retroperitoneal and intraabdominal fat. As with MRCP, these sequences may be performed as multiple thin slices that can be postprocessed or as a thick slab performed in multiple projections (Fig. 2.48). Breath-hold sequences are preferable to free-breathing sequences. However, for patients unable to hold their breath, respiratory triggering is helpful to reduce motion artifact. Images should be obtained in the coronal plane with a large field of view that includes the entire collecting system. As with conventional IVU, oblique imaging of the intrarenal collecting systems may be helpful to better define anatomy. Although static MR urography is effective in depicting obstructed urinary tracts, nondistended collecting systems may be difficult to portray. If necessary, this problem can be mitigated by hydrating the patient before the examination and administering a low dose of furosemide. An advantage of static MR urography over contrast-enhanced techniques is that it is independent of renal function and eliminates the need for delayed imaging to define the level of ureteral obstruction. Therefore, static MR urography may be more time efficient than excretory urography in this setting.
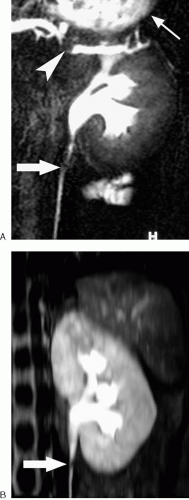
Excretory MR urography using an intravenous gadolinium chelate is an alternative strategy for imaging the renal collecting systems (Fig. 2.49). This is most often performed as an adjunct to a contrast-enhanced MRI performed for other reasons. However, specific indications for performing contrast-enhanced MR urography include preoperative localization of nondistended ureters or demonstration of a communication between the renal collecting system and a cystic structure or fluid collection (Fig. 2.50). The feasibility of MR renography, in which renal function is quantified with gadolinium-enhanced dynamic MRI, has been demonstrated (1). However, this technique is not widely used.
MR urographic techniques are still evolving. The optimal intravenous contrast dose, method of administration, sequence parameters, and timing of image acquisition for excretory MR urography have yet to be determined. A simple test dose of 1 to 2 mL of contrast material often provides a useful MR urogram on subsequent coronal T1-weighted three-dimensional (3D) gradient echo sequences, as long as sufficient time has elapsed to allow the contrast material to enter the collecting systems (Fig. 2.51). However, this low-dose method may be limited by incomplete ureteral visualization due to inadequate patient hydration (2).
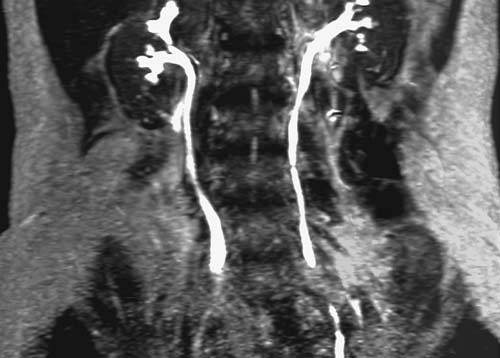 FIG. 2.51. Low-dose MR urogram. Coronal maximum intensity projection image created from three-dimensional gradient echo sequence performed 5 minutes after 2-mL dose of intravenous gadolinium. |
The use of a standard 0.1-mmol/kg dose of gadolinium chelate often results in signal loss within the renal collecting systems due to the T2 shortening effect of gadolinium at high concentrations (Fig. 1.32). This T2 shortening effect of gadolinium is one reason that MR urograms using T2-weighted techniques are commonly performed before gadolinium administration (Fig. 1.35). Hydrating the patient and administering a low dose of diuretic such as furosemide (typically 5 to 10 mg) prevents excessive concentration of the contrast material within the collecting systems while improving ureteral distention and contrast distribution in patients without obstruction (3). Gadolinium-based contrast agents have a higher specific gravity than urine and layer dependently within the renal collecting systems and bladder if undisturbed. Turning a supine patient prone or rolling the patient from side to side may alleviate this problem. The infusion of normal saline may augment the effects of furosemide or serve as a standalone
method of improving gadolinium dilution and distribution. However, neither the optimal gadolinium dosage nor the role of saline infusion in MR urography has been thoroughly established. Excretory MR urography is unlikely to succeed in patients with severely compromised renal function, and saline infusion is not recommended for fluid-restricted patients.
method of improving gadolinium dilution and distribution. However, neither the optimal gadolinium dosage nor the role of saline infusion in MR urography has been thoroughly established. Excretory MR urography is unlikely to succeed in patients with severely compromised renal function, and saline infusion is not recommended for fluid-restricted patients.
3D gradient echo sequences, preferably combined with fat suppression, provide high-resolution MR urographic images following gadolinium administration that can be used to create maximum intensity projections in multiple views. The coronal plane provides the greatest anatomic coverage in the shortest time, although additional planes may occasionally be useful. If coronal images are of sufficiently high resolution with nearly isotropic voxel dimensions, multiplanar re-formations may substitute for additional acquisitions in other planes. High-performance imaging gradients are necessary to allow complete image acquisition within a single breath-hold.
Although maximum intensity projection and multiplanar re-formation are the most common display methods for MR urography, occasionally other novel reconstruction techniques may be beneficial. For example, virtual cystoscopy or ureteroscopy may be performed using high-resolution, 3D fast spin echo data sets (Fig. 2.52). As with static MR urography, virtual cystoscopy using T2-weighted images must be performed before administration of intravenous gadolinium.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree