Magnetic Resonance Cholangiopancreatography
The refinement and dissemination of magnetic resonance cholangiopancreatography (MRCP) techniques have revolutionized evaluation of the biliary tree and pancreatic duct. MRCP has proven particularly useful in patients for whom endoscopic retrograde cholangiopancreatography (ERCP) is contraindicated, technically difficult, or incomplete. When combined with standard abdominal imaging sequences, MRCP provides a complete assessment of the abdomen not possible with endoscopic techniques.
Technique
Most MRCP techniques use heavily T2-weighted sequences, which exploit the long T2 relaxation time of fluid. Background suppression results from the T2 decay of non-fluid-containing structures, which have shorter T2 relaxation times than fluid. The additional application of fat suppression further suppresses background signal, improving the conspicuity of ductal structures. MRCP images may be acquired as a single thick slab using a single-shot fast spin echo sequence or as a series of thin slices that can be reconstructed via the maximum intensity projection (MIP) algorithm (Fig. 2.29). Data acquired as a thick slab cannot be manipulated to create multiple views. Therefore, thick-slab MRCP techniques require the acquisition of multiple separate projections. Even though thin slice techniques overcome this limitation by allowing multiplanar three-dimensional (3D) reconstructions of acquired data, such reconstructions are potentially limited by respiratory motion-induced slice misregistration. Because most MRCP sequences can be performed in less than 30 seconds on newer scanners, both techniques can be routinely used to capitalize on the advantages of each method.
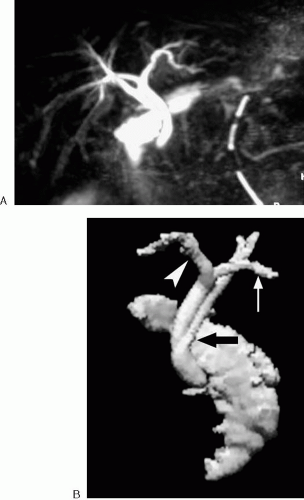
A thick-slab, single-shot fast spin echo sequence with a very long effective echo time (TE) provides a useful overview of the ducts. At a minimum, coronal and bilateral oblique projections should be performed with thick-slab techniques. A slab thickness of 4 to 8 cm generally provides adequate coverage and minimizes overlap from other fluid-containing structures. Thin section images (2 to 4 mm) can be easily obtained with a HASTE sequence in the coronal (or oblique coronal) and axial planes. With this sequence, the entire biliary and pancreatic ductal systems can be covered in one or two breath-holds. Some magnetic resonance imaging (MRI) scanners can perform a 3D respiratory-triggered fast spin echo sequence with extremely thin partitions or slices. When successful, such acquisitions enable very fine 3D reconstructions (Fig. 2.30). However, these sequences are relatively time consuming and easily degraded by inconsistent breathing. Therefore, we do not perform a respiratory-triggered sequence when the breath-hold images are diagnostic.
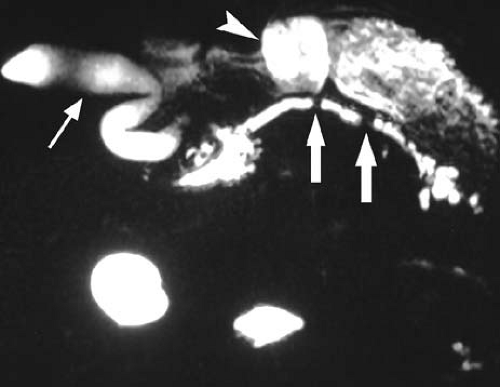
A successful MR practitioner takes advantage of the infinite multiplanar capability of MRI. For thick-slab imaging, an oblique axial view of the pancreatic or intrahepatic bile ducts is often helpful in delineating anatomy obscured in other planes. Thin slices obtained parallel or perpendicular to a duct of interest may be helpful to confirm the presence of an intraductal stone or demonstrate a communication between the duct and a cystic structure. MRCP sequences take relatively little time to perform, and creativity in choosing imaging planes is often rewarded with informative data (Fig. 2.31).
Negative oral contrast agents may be helpful to suppress the signal from the stomach, duodenum, or other fluid-filled loops of bowel that overlap the biliary or pancreatic ducts. However, the use of negative oral contrast agents is usually unnecessary for diagnostic purposes. Furthermore, visualization of the duodenum is often desirable, because it allows one to localize the position of the ampulla and accurately determine the presence and length of a biliary or pancreatic duct obstruction or stricture.
The use of secretin has been studied for use with MRCP of the pancreatic duct (1,2,3,4). Secretin is a hormone produced by the duodenum that stimulates pancreatic secretion in response to acidic contents from the stomach. When administered as part of an MRCP examination, secretin enhances visualization of the pancreatic duct and has been successfully used in the assessment of exocrine reserve in chronic pancreatitis. A synthetic form of secretin has recently been approved for clinical use in the United States.
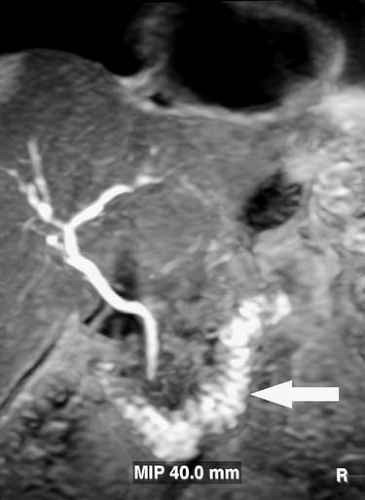
Hepatobiliary contrast agents, such as mangafodipir (Teslascan), offer an alternative technique for visualizing the bile ducts (Fig. 2.32). These agents are taken up by hepatocytes and are partially excreted in the bile. The time from intravenous administration to appearance of the contrast agent in the bile varies with hepatic function. However, timing of the acquisition is not critical, in that contrast may be excreted in bile for several hours after injection. For mangafodipir-enhanced MR cholangiography, we typically begin imaging the bile ducts with a high-resolution 3D gradient echo sequence approximately 15 to 30 minutes after injection. Currently, mangafodipir remains the only approved hepatobiliary agent for clinical use in the United States.
Kinematic MRCP may be useful in distinguishing biliary dilatation caused by an obstructing ampullary or periampullary lesion from nonobstructive causes of biliary dilatation. This assessment can be performed by repeatedly imaging through the sphincteric segment of the distal common bile duct in the oblique coronal plane using a heavily T2-weighted thick-slab (2 to 3 cm), single-shot fast spin echo or HASTE sequence (5,6).
Clinical Applications
Biliary Applications
Preoperative Imaging
MRCP clearly demonstrates biliary anatomy in most patients. Therefore, MRCP has become a useful adjunct to standard MRI of the liver performed as part of the preoperative assessment of patients with liver tumors and for evaluation of potential living-related hemiliver donors (7,8). In the assessment of living-related donors, complete visualization of the
relevant intrahepatic bile ducts can be achieved in approximately 90% of individuals. However, smaller or more peripheral branches may elude detection in some individuals. Hepatobiliary agents such as mangafodipir may alleviate this problem by better demonstrating small intrahepatic radicles (9,10).
relevant intrahepatic bile ducts can be achieved in approximately 90% of individuals. However, smaller or more peripheral branches may elude detection in some individuals. Hepatobiliary agents such as mangafodipir may alleviate this problem by better demonstrating small intrahepatic radicles (9,10).
Congenital Biliary Anomalies
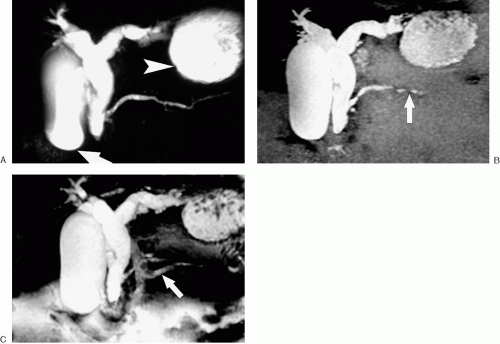
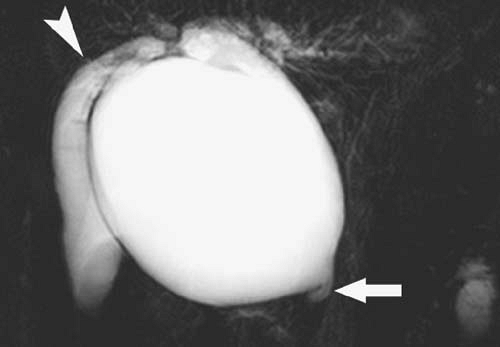
Choledochal cysts (Fig. 2.33) are congenital biliary dilatations thought to result from anomalous union of the common bile and pancreatic ducts, allowing reflux of pancreatic enzymes into the bilary tree. MRCP may be useful for establishing the diagnosis of choledochal cyst and for demonstrating anomalous pancreaticobiliary ductal union, although the latter finding may prove more difficult to demonstrate (11,12,13).
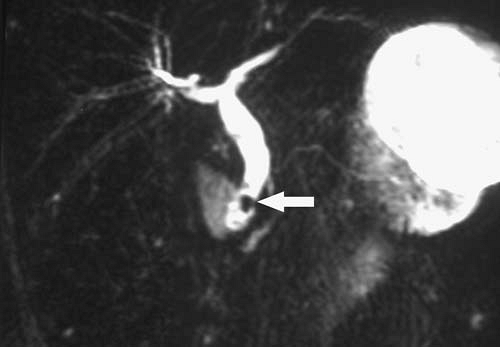
Choledocholithiasis
Choledocholithiasis (Fig. 2.34) remains one of the most common indications for MRCP of the biliary system. The sensitivity and specificity of MRCP for the diagnosis of choledocholithiasis are approximately 91% to 98% and 89% to 98%, respectively (14,15,16,17). Because MRCP does not rely on retrograde injections of contrast material to visualize ducts, it may be more sensitive than ERCP for the diagnosis of intrahepatic bile duct stones (18).
Trauma
Traumatic injury of the biliary system may result from blunt or penetrating abdominal trauma or surgical intervention. Conventional MRCP may demonstrate disruption of a bile duct, although T2-weighted images alone cannot reliably distinguish between a biloma and other fluid collections. Preliminary evidence suggests that hepatobiliary agents such as mangafodipir may be useful in the diagnosis and characterization of bile leaks and bilomas (Fig. 2.35) (19).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree