family history, age, male gender)
• Generally affects older patients
• Patients often have concomitant essential hypertension, CKD, congestive heart failure, stroke, or myocardial infarction (MI)
• Typically proximal or ostial (at origin from aorta)
■ Pathophysiology:
■ Renal artery stenosis is an anatomic finding that can lead to renovascular hypertension or ischemic nephropathy or both. In unilateral renal artery stenosis, the affected kidney secretes renin leading to hypertension, which causes pressure natriuresis in the contraleral kidney and consequent hypovolemia. In bilateral renal artery stenosis, patients are hypervolemic because there is no contralateral natriuresis; although plasma renin levels are usually normal, these levels can be considered higher than expected given that hypertension and hypervolemia are present (Fig. 15.1A, B) (Pickering, 1989).

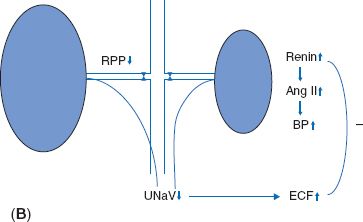
FIGURE 15.1 A: Unilateral renal artery stenosis. B: Bilateral renal artery stenosis (RPP = renal perfusion pressure; Ang II = angiotensin II; BP = blood pressure; UNaV = urinary sodium excretion; ECF = extracellular fluid.)
■ In ischemic nephropathy, CKD develops due to impaired renal blood flow, leading to nephrosclerosis/glomerulosclerosis. Recurrent cholesterol emboli from atherosclerotic plaques may contribute to injury in the atherosclerotic form.
■ Antihypertensive medications lead to a decrease in BP, which, in the presence of renal artery stenosis, results in decreased afferent arteriolar pressure and a drop in glomerular filtration rate (GFR). RAS blockers such as angiotensin-converting enzyme (ACE) inhibitors (ACEIs) and angiotensin receptor blockers cause efferent arteriolar dilatation, thus further decreasing GFR (Fig. 15.2A, B). A marked fall in GFR when RAS blockers are begun should raise suspicion for RAS.
■ Diagnosis:
■ Plasma renin activity: Not helpful, as it is inadequately sensitive and specific and is affected by antihypertensive medications
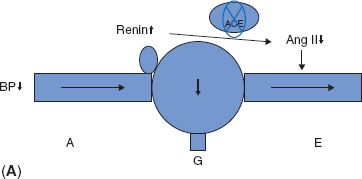
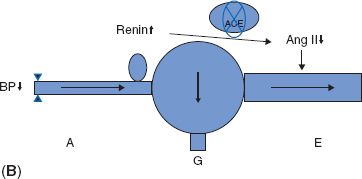
FIGURE 15.2 A: Inhibition of RAS dilates efferent arterioles and lowers glomerular capillary pressure. B: In the presence of renal artery stenosis, there is a greater drop in glomerular capillary pressure after RAS inhibition (A = afferent arteriole; G = glomerulus; E = efferent arteriole.)
■ Renal vein renin sampling: Classic test; an increase in renin from the affected kidney with contralateral renin suppression is expected with unilateral stenosis; however, difficult to interpret with bilateral stenosis; invasive; now rarely performed (Simon & Coleman, 1994)
■ ACEI -augmented renal scintigraphy: The fall in GFR in the affected kidney is detected; can predict response to intervention; however, now performed rarely (Taylor, 2000)
■ Doppler ultrasound: Compares peak systolic velocity of the renal arteries (stenosis leads to an increase in velocity); operator-dependent; in some centers, it is screening procedure of choice (Olin et al., 1995; Radermacher et al., 2001)
■ Magnetic resonance angiography (MRA) (with or without gadolinium): Requires breath holding, long scan times, and may be uncomfortable for patients with claustrophobia; gadolinium contrast contraindicated with severe CKD (eGFR <30 mL/min/1.73 m2) or end-stage kidney disease (ESKD). Contraindicated in some patients (i.e., pacemakers, metal vascular clips) and hard to interpret in patients with previous stents (Cheung et al., 2006)
■ Computed tomography (CT) angiography with contrast: Best for fibromuscular dysplasia; can involve substantial contrast load (Olbricht et al., 1995)
■ Selective angiography: Gold standard, but invasive. Advantages are that it can measure pressure gradient and allow for immediate intervention with angioplasty ± stent
■ Surgery: Risks include bleeding, infection, MI, cerebrovascular accident (CVA), atheroembolism, and acute renal failure. Mortality is 1% to 6%. Excellent patency. Now rarely done in most centers
■ Percutaneous transluminal angioplasty (PTA): Procedure of choice for fibromuscular dysplasia. It can be repeated if stenosis recurs. Stenting is not used in fibromuscular dysplasia since PTA provides up to 100% cure rate.
■ Stent placement—Stenting is appropriate for atherosclerotic renal artery stenosis because it maintains patency despite elastic recoil. Definite indications include (1) poor response to PTA, (2) early restenosis after angioplasty, and (3) renal artery dissection. However, the benefits of peripheral revascularization comes with risks as well; in atherosclerotic renal artery stenosis, the likelihood of cure is variable and there is widespread variability in the reporting of outcomes (Ives et al., 2003). A major clinical trial of stenting versus medical therapy in atherosclerotic renal artery disease is currently being performed (Cooper et al., 2006).
■ Medical therapy: Control diabetes, control lipids, and maximally manage coronary artery disease
• Fibromuscular dysplasia: Medical therapy is inferior to intervention
• Atherosclerosis: Control BP and risk factors for CVA and MI (antiplatelet drugs, statins, smoking cessation); need to follow serum creatinine as otherwise unexplained progressive renal insufficiency warrants consideration for intervention
RENAL ARTERY EMBOLISM
■ Presentation: Variable with abdominal pain, gross hematuria, flank tenderness, fever, and hypertension. Anuria is present in bilateral renal thromboembolism and solitary kidney with renal thromboembolism
■ Etiology: The most common cause is atrial fibrillation, which is known to be associated with a four- to sevenfold higher risk of peripheral emboli. Renal thromboembolism constitutes 2% of peripheral emboli caused by atrial fibrillation. Other causes include bacterial endocarditis, heart tumors, mural thrombus (dilated cardiomyopathy), repair of aortic aneurysms, and revascularization of renal artery stenosis (Cheng et al., 2003)
■ Laboratory:
■ Elevated lactate dehydrogenase (LDH), aspartate aminotransferase (AST) (renal infarction)
■ Hematuria
■ Decreased urinary sodium (due to renal hypoperfusion)
■ Diagnosis:
■ CT with contrast will demonstrate lack of kidney enhancement. However, the use of contrast carries with it the risk of renal failure.
■ Magnetic resonance imaging (MRI) will usually visualize renal arteries. However, MRA with gadolinium may be necessary for visualization (note that gadolinium is contraindicated with GFR <30 mL per minute).
■ Renal isotopic flow scans will demonstrate absent or reduced perfusion.
■ Doppler ultrasound studies are generally not useful.
■ Angiography is the gold standard but is invasive; this is only used if intervention is contemplated. Again, the use of contrast carries with it the risk of renal failure.
■ Kidneys can tolerate lack of blood flow for only 60 to 90 minutes without tubular injury. In the absence of collateral circulation (which is typical of renal artery embolism), prolonged ischemia results in renal infarction.
■
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


