Chapter 3.10
Lymphangiectasia and nutrition
Anu Paul and Ashish P. Desai
King’s College Hospital NHS Foundation Trust, London, UK
Intestinal lymphangiectasia is a rare digestive disease that causes protein loss from the intestine. It is characterised by diffuse or localised dilation of the intestinal lymphatics and stasis of the lymph contained within. This eventually leads to rupture of the lymph vessels, resulting in loss of lymphatic fluid into the lumen of the intestine.
The term ‘intestinal lymphangiectasia’ was first coined in 1961 by Waldmann and associates. They described 18 cases of idiopathic hypercatabolic hypoproteinemia characterised by low serum albumin and gammaglobulins with high faecal albumin and intestinal biopsies showing dilated lymph vessels [1].
Lymphangiectasia of the intestine may be primary or secondary. Primary intestinal lymphangiectasia is a congenital malformation that usually presents before 3 years of age. Secondary intestinal lymphangiectasia usually occurs as a consequence of increased lymphatic pressure caused by obstruction to the lymphatics or increased venous pressure. It can be seen in syndromes such as Hennekam’s syndrome [2], Turner’s syndrome, aplasia cutis congenita, von Recklinghausen’s syndrome, Klippel–Trenaunay syndrome [3] and Noonan syndrome [4].
3.10.1 Embryology
The progenitors of the lymphatic system are believed to arise from the endothelial cells of the embryonic venous structures [5]. These cells differentiate and express molecular markers that distinguish them from venous cells. These specific cells then attain autonomy from the venous system by budding and peripheral migration. This may be the reason why many lymphatic abnormalities are also associated with malformations of the vascular system.
At a molecular level, the initial signalling molecule responsible for lymphangiogenesis has not been identified. Vascular endothelial growth factor (VEGF) is a key molecular regulator of endothelial proliferation and migration. The VEGF family includes five isotypes: A, B, C, D and E. The isotypes VEGF-C and VEGF-D and their cognate receptor VEGFR-3 represent the first and best studied of the lymphatic specific signalling mechanisms [6].
3.10.2 Functions of the lymphatic system
The lymphatic system provides a system of mass transport parallel to blood circulation in the human body as well as playing a role in water and nutrient absorption. Large biomolecules suchw as enzymes and hormones are transported from their site of synthesis to the blood circulation by means of lymphatic transport. The lymphatic system also ensures absorption of excess fluid and protein from the interstitial space. Thus it is very important for the homeostasis of interstitial fluid [7].
From a nutritional perspective, the main role of the lymphatic system is in the transport of lipids, mainly triglycerides and long-chain fatty acids from the intestine. Ingested lipids are emulsified by bile and digested by lipase to produce monoglycerides and fatty acids. Short- and medium-chain fatty acids can be absorbed directly into the blood circulation. The long-chain fatty acids and monoglycerides are absorbed into enterocytes where they undergo re-esterification to form triglycerides. The triglycerides are aggregated into chylomicrons and actively transported out of the enterocyte into the interstitial space, from where they are passively absorbed in the lacteals and transported in the lymph.
The lymphatic system also has a major role to play in immune trafficking. The lymph nodes strategically placed along the lymph vessels are able to sample the lymph and perform immunological surveillance of the interstitial space [7].
3.10.3 Aetiopathogenesis of intestinal lymphangiectasia
Intestinal lymphangiectasia occurs due to abnormal development of the lymphatic system with dilated lymphatics in the lamina propria of the small intestine [1]. The exact aetiology of intestinal lymphangiectasia is unknown. It is postulated that it may be due to altered expression of the regulator molecules that control lymphangiogenesis such as VEGFR-3. Other regulatory molecules such as Prospero homeobox1 (PROX1), forkhead box C2 (FOXC2) and sex determining region (SRY) Y box 18 (SOX18) may also have a role to play [8].
Nutritional causes
After a meal rich in long-chain fatty acids, lymphatic flow in the lacteals and intestinal lymphatics is known to increase. This promotes further engorgement and dilation of the affected lymphatics in primary intestinal lymphangiectasia, causing them to rupture. Loss of valuable lymph containing proteins and lymphocytes then ensues, leading to protein-losing enteropathy and malabsorption.
3.10.4 Clinical features
Many clinical features of intestinal lymphangiectasia can be attributed to protein-losing enteropathy and malabsorption. The classic triad of features includes lymphocytopenia, hypoalbuminaemia and hypogammaglobulinaemia. This manifests most usually as bilateral lower limb lymphoedema. In extreme cases, oedema may involve the face or scrotum. Effusions may develop in the pleural, pericardial or peritoneal spaces (Figure 3.10.1). This may be accompanied by abdominal pain, inability to gain weight and deficiency of fat-soluble vitamins. Due to impaired fat absorption, steatorrhoea is a presenting feature. Macular oedema can be seen in extreme cases, leading to blindness [9].
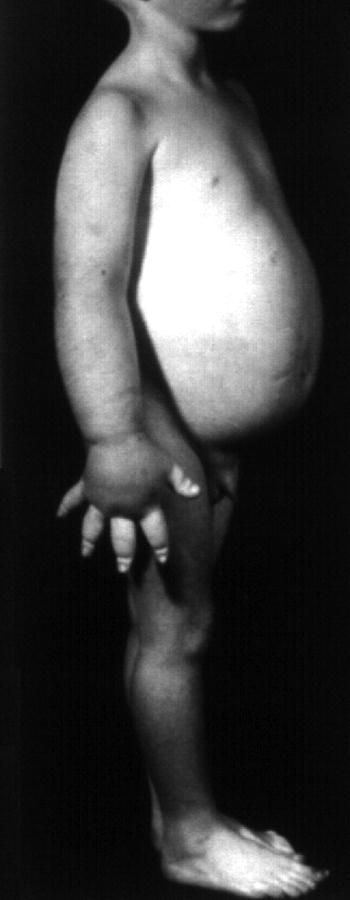
Figure 3.10.1 Patient profile before starting treatment. Reproduced with permission from Dr Babu Vadamalayan, King’s College Hospital, London.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





