Fig. 13.1
The newer da Vinci Xi (a) and previous generation (b), systems are seen here. The Xi offers greater flexibility with overhead instrument arm location and the ability to operate in all abdominal quadrants without repositioning the robot. With permission from Intuitive Surgical, Sunnyvale, CA
The technical approaches may include either a fully robotic or a hybrid operation. In the hybrid technique, the colorectal vasculature is ligated and the colon mobilized prior to docking the robot. In a completely robotic approach, ligation of vasculature, colonic, and rectal mobilization is completed entirely with the robot.
In the hybrid technique, the patient position may be easily changed to aid the dissection prior to robot docking. Once the laparoscopic mobilization is completed, the patient is placed in steep Trendelenburg and leveled in the horizontal plane or a slight right-side-down tilt. The robot can be docked either between the patient legs for the pelvic dissection in a non-reconstructive operation or over the left hip for a reconstructive operation in which access to the perineum is required. When performing a totally robotic dissection, the robot is docked over the patient’s left hip after the patient is placed in Trendelenburg with the right side tilted downward. It is helpful to have adequate exposure of the colon, splenic flexure, and pelvis simultaneously as the patient bed may not be repositioned with the robot docked. Too steep Trendelenburg will make visualizing the splenic flexure and transverse colon difficult and too steep right-side tilt may inhibit visualization of the pelvis. In such situations, the robotic arms may be disengaged, the bed appropriately adjusted, and the arms re-engaged.
13.2.2 Trocar Placement
Abdominal access can be obtained by a variety of methods. We prefer the use of a modified open technique, utilizing an Optiview ® trocar (Ethicon Endo-Surgery, Inc.) placed under direct visualization in the midline just superior to the umbilicus. The Optiview® trocar has particular benefit in an obese patient in which a traditional open technique is difficult secondary to poor visualization. Ideally, the 30-degree camera is positioned roughly 15 cm from the target anatomy and is positioned at a 30-degree down angle. It is critical with older S and Si models that the working arms are positioned outside this camera cone area, which is the visual field of the camera based on the target anatomy. Additional trocars are placed once insufflation is achieved to ensure the appropriate 8–10 cm distances between ports for S and Si system and 6–8 cm for the Xi system to avoid external or internal collisions.
In the hybrid technique we generally place 4 additional trocars (Fig. 13.2a). Robotic trocars are placed in the right and left lower quadrants (arms 1 and 2, respectively), approximately at the midclavicular lines. Another robotic trocar (arm 3) is placed in the left lateral abdomen, cranial to both the anterior superior iliac spine and arm 2. An additional 5-mm trocar (assistant port) is placed in right upper quadrant.
Fig. 13.2
(a) Trocar positions for a hybrid robotic approach and (b) trocar positions for a completely robotic approach. With permission from Intuitive Surgical, Sunnyvale, CA
Port placement differs slightly in the completely robotic technique. Abdominal access is obtained in the same position and manner as previously described. Robotic instrument ports (arms 1 and 2) are placed in similar positions. A robotic trocar (arm 3) is placed in the left lateral abdomen, just superior to anterior iliac spine. A similar trocar is placed for the third arm in the right upper quadrant just to the right of midline—this position is used for the splenic flexure. The robot should be positioned over the left hip such that a straight line drawn from the midpoint of the camera arm attachment crosses the anterior superior iliac spine. The most distal aspect of the camera arm and port should be in line with the patient’s spine. It is critical that the alignment of arm 1 and the camera is not in the identical vector toward the left colon and splenic flexure, as this position would impede mobilization and dissection (Fig. 13.2b).
Issues that are critical to consider include the distance to the target anatomy and the potential for the boney aspects of the pelvic sidewall and sacral promontory to impede surgical dissection. For example, the monopolar scissors is 57 cm in length with a working length of 27 cm from the remote center to tip. Trocars placed too far cephalad in a patient with a long torso will make the presacral dissection toward the pelvic floor difficult secondary to reach. Likewise, the sacral promontory acting as a fulcrum can lead to a poor angle of dissection into the presacral space. Finally, trocars placed too far laterally (particularly in a male patient) will make the low pelvic dissection difficult secondary to collisions with the lateral pelvic sidewall.
13.2.3 Operative Technique
13.2.3.1 Step 1: Initial Exposure
The greater omentum should be reflected over the transverse colon toward the liver and the small bowel retracted out of the pelvis into the right upper quadrant. In a female patient, it may be necessary to suspend the uterus to obtain an unobstructed view into the deep pelvis. We place a suture transabdominally around the round ligaments to suspend the uterus anteriorly or directly through the fundus of the uterus. Alternatively, a uterine manipulator may be placed transvaginally to suspend the uterus and vagina away from the rectum to allow easier dissection in the rectovaginal septum.
13.2.3.2 Step 2: Control of the Inferior Mesenteric Artery and Inferior Mesenteric Vein
Depending on the length of colon needed, vessel ligation may include any combination of inferior mesenteric artery (IMA), proximal or distal to the left colic artery, as well as inferior mesenteric vein (IMV) ligation. Whether this particular portion of the operation is done with traditional laparoscopic techniques or robotic techniques, the principles remain the same. If being completed laparoscopically, the patient is placed in steep Trendelenburg; the assistant grasps the rectosigmoid junction and retracts the rectum superiorly out of the pelvis. Robotically, a monopolar-curved scissors is initially used in arm 1 (right lower quadrant) and a fenestrated bipolar forceps used in arm 2 (left lower quadrant); a double-fenestrated atraumatic bowel grasper is placed in arm 3 (left lateral abdomen). Using arm 3, the rectosigmoid junction is grasped and the rectum is placed on tension proximally, pulling it out of the pelvis. Alternatively, an assistant may grasp this area, allowing arm 3 to grasp more distally on the rectum to provide additional traction, placing the rectosigmoid mesocolon and mesorectum on tension. It is critical that the upper rectum be elevated in such a way as to stretch the peritoneum overlying the right pelvic gutter, as well as the superior rectal artery to help separate the vessels from the sacral promontory. Electrocautery is then utilized to incise the peritoneum along the right side of the rectum, caudal to the sacral promontory. This exposes and opens the presacral space (Fig. 13.3a, b).
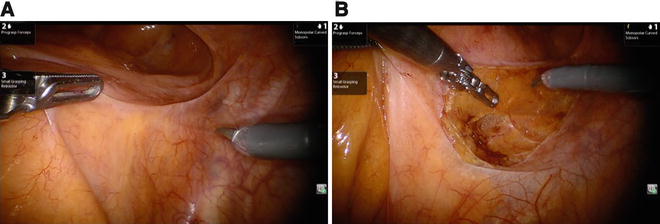
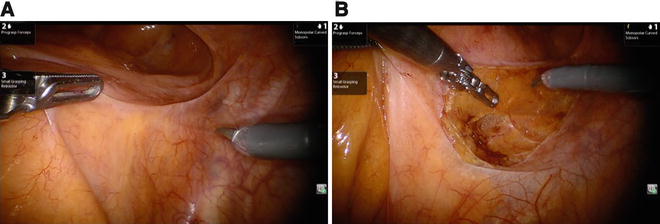
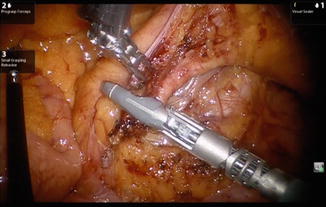
Fig. 13.3
(a, b) An unobstructed view of the pelvis is obtained. The rectum is retracted cephalad and to the left using arm 3. The rectum must be elevated to stretch the peritoneum and raise the superior rectal artery anteriorly to separate the vessels from the sacral promontory. Electrocautery is then used to incise the peritoneum along the right side of the rectum, caudal to the sacral promontory
Dissection is carried cephalad along the posterior aspect of the mesorectum toward the IMA (Fig. 13.4a), taking care not to breach the fascia propria of the rectum and avoiding injury to the superior hypogastric nerves. Injury to the nervous structures around the IMA may result in retrograde ejaculation and/or bladder dysfunction. As one dissects directly below the superior rectal artery and above the retroperitoneal fascial planes, the left ureter and gonadal vessels should be identified just above the pelvic brim. As this dissection continues in this plane, the vessel is elevated from the retroperitoneum and the ureter and gonadal vessels can be easily swept bluntly posteriorly to maintain their position within the retroperitoneum, posterior and lateral to the IMA (Fig. 13.4b).
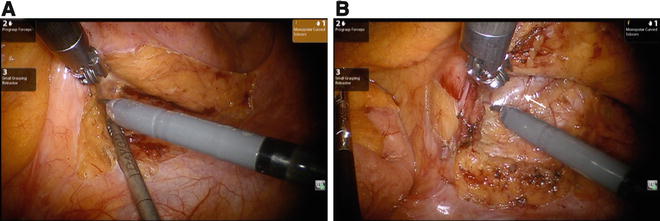
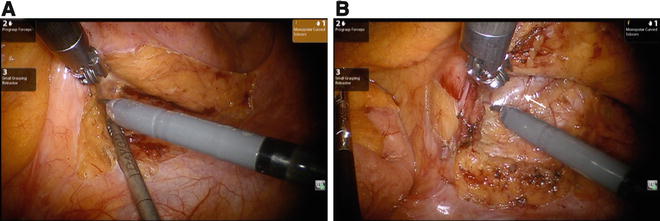
Fig. 13.4
(a, b) Identifying and isolating the inferior mesenteric artery—dissection is carried cephalad along the posterior aspect of the mesorectum toward the IMA. Arm 2 (LLQ) is placed posterior to the vascular bundle and mesorectum and retracted anteriorly. The assistant may place countertraction using either a laparoscopic grasper or suction device to aid the dissection. The vessel is elevated from the retroperitoneum, and the gonadal vessels and ureter (white arrow) should be identified within the retroperitoneum, just above the pelvic brim, posterior and lateral to the IMA
While there is no oncologic benefit to high versus low ligation of the IMA, we prefer to ligate this vessel at its origin to obtain maximal length for a potential low pelvic anastomosis and to minimize tension [8]. Once the IMA is isolated at its origin, we ligate this using either a 5-mm blunt tip LigaSure (Covidien Surgical Solutions, Mansfield, MA) vessel sealer or the da Vinci® EndoWrist® One™ vessel sealer (Intuitive Surgical Inc., Sunnyvale, CA) (Fig. 13.5). Other methods of vascular control include the use of endoscopic staplers, clips, or sutures. The colonic mesentery can now be elevated off the retroperitoneum proximally and laterally. If in the correct plane, much of this dissection can be carried out bluntly. The extent of dissection is superior to the inferior border of the pancreas and laterally overlying the Gerota’s fascia. The cut edge of the colonic mesentery can continue to be transected superiorly, lateral to the duodenum to include the IMV. If the IMV cannot be reached in this manner, it may be transected prior to releasing the splenic flexure.