Fig. 14.1
Admission CT scan of a 39-year-old man, after hepatorrhaphy, with an extensive injury to the right liver. Right hepatic artery clipping and tube cholecystostomy were previously done at another hospital of the national health system network
At our institute he underwent median relaparotomy with extension to the right renal flap. We then removed roughly two liters of blood clots and found no evidence of active bleeding. Liver resection was planned by a multidisciplinary team and was aimed at excision of the gallbladder and the right lobe of the liver.
After sectioning of the falciform ligament and of the triangular ligament and right coronary, we performed a skeletonization of the retrohepatic IVC with ligature and sectioning of accessory veins. We then isolated the right hepatic vein and proceeded to isolate and section the cystic duct and cystic artery for retrograde cholecystectomy. Subsequently, we isolated the right branch of the portal vein and the right branch of the hepatic artery, which was divided between ligatures after the removal of the two metal clips from the anterior branch of the right hepatic artery.
The right branch of the portal vein and the right hepatic vein were then severed with a vascular stapler. After the intraparenchymal sectioning and cutting of the right branch of the bile duct, we proceeded to parenchymal transection with the aid of electrocautery, ultrasonic dissector, and stapler (Fig. 14.2).


Fig. 14.2
Remnant hepatic parenchyma after right hemiliver resection. An intraoperative ultrasound was done to confirm valid flows to and from the left liver
One of the most relevant indications for anatomic hepatic resection in this case was the previous, inappropriate surgical treatment performed at the referring facility. Hepatorrhaphy by simple catgut suture and Spongostan application (Fig. 14.3) was less than ideal. For bailout first surgical approach, we suggest suture, supported by Teflon felt (DuPont Pharmaceuticals, Wilmington, DE), Fig. 14.4, and perihepatic packing.
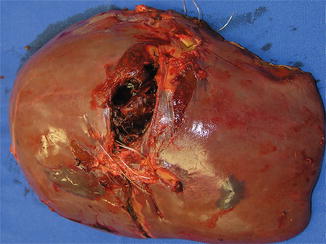
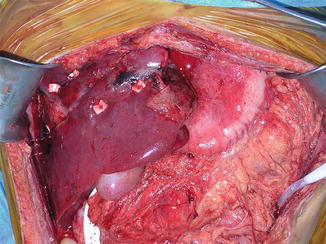
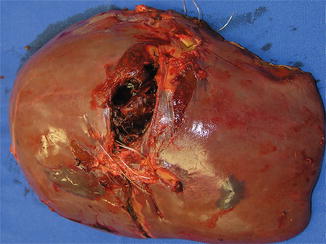
Fig. 14.3
Surgical specimen after right hepatectomy; of note is the previous surgical hepatorrhaphy for managing the liver fracture by simple suture with chromic catgut
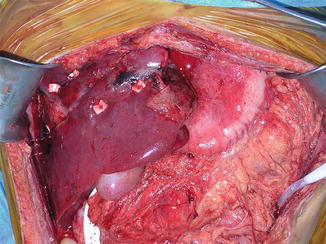
Fig. 14.4
Complex fracture of the right liver segments that was treated with hepatorrhaphy; the Teflon felts were adjuvant for supporting liver suture line fields
An intraoperative ultrasound was performed to confirm valid blood flow to and from the left liver. Intraoperative cholangiography confirmed the patency of the left bile duct. Overall blood loss was 450 mL and operating time was 365 min. The postoperative course was complicated by mild biliary leakage, which was treated and resolved with ERCP and metallic stent placement (Fig. 14.5). The patient was discharged home on postoperative day 13. At present, he is alive and well. An uneventful ERCP and biliary stent removal was done 2 months after surgery, with no complaints (Fig. 14.6).



Fig. 14.5
Postoperative cholangiography confirmed mild output biliary leakage. At ERCP a metallic stent was placed (as evidenced in the rectangle box)

Fig. 14.6
Follow-up cholangiography, 2 months after surgery for liver injury, showing resolution of the biliary leakage
Conclusion
Technical skills in advanced hepatobiliary surgery, patient hemodynamic and resuscitation, diagnostic evaluations, operative indications by grade of injury, selection criteria for operative management, and criteria for the choice of operation are mandatory for indicating formal liver resection as initial or delayed management of patients with complex liver trauma.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








