Ligation of Bleeding Ulcer, Antrectomy, Vagotomy, and Gastrojejunostomy
Bruce Schirmer
Bleeding duodenal ulcer is a surgical emergency that has decreased in frequency over the past several decades due to the overall decrease in the incidence of peptic ulcer disease. However, the condition still arises and is a life-threatening one for the individual who develops it. Surgery remains an important treatment option for the patient with a bleeding duodenal ulcer. Its role has been decreased from primary line therapy in most situations to secondary treatment when the patient is stable enough to undergo less invasive therapy, in particular flexible endoscopic attempts to relieve the bleeding.
Indications
Specific indications for the performance of antrectomy, vagotomy, gastrojejunostomy, and oversewing of a bleeding duodenal ulcer are as follows:
Initial treatment of a patient with a bleeding duodenal ulcer causing hemodynamic changes unresponsive to intravenous fluid and blood product transfusion.
Treatment of a patient with bleeding duodenal ulcer who has failed attempts at endoscopic therapy to control the bleeding ulcer and for whom interventional angiographic therapy to control the bleeding is either unavailable, has failed, or is felt to be contraindicated.
Treatment of a patient with bleeding duodenal ulcer for whom no endoscopic or radiographic therapeutic options to arrest the bleeding are available.
In addition to the above three indications for the operation, the following parameters are also considered important by many surgeons to be present to warrant this operation:
The patient should have had a history of previous peptic disease to warrant resectional therapy.
The previous peptic disease should not have been so severe as to render the pyloric and postpyloric area severely scarred.
The patient’s condition in the operating room must be one of hemodynamic stability once the bleeding ulcer has been oversewn.
Contraindications
Specific contraindications for the performance of antrectomy, vagotomy, gastrojejunostomy, and oversewing of a bleeding duodenal ulcer are as below. This list may not be totally comprehensive but should encompass the major contraindications.
Hemodynamic instability in the operating room necessitating the performance of the most rapid operation feasible (vagotomy, pyloroplasty, and oversewing of the ulcer).
Severe scarring of the pyloric and proximal duodenum, such that the resection staple line for the distal margin of the antrectomy would be at jeopardy for breakdown.
No previous history of peptic disease or potential other etiologies (e.g., aspirin or nonsteroidal anti-inflammatory drug ingestion) that may have contributed to the ulcer diathesis.
Previous antireflux surgery, placement of lap-adjustable band for weight loss, or other operation with extensive dissection around the gastroesophageal junction which would contraindicate easy performance of a truncal vagotomy.
The overwhelming issue regarding preoperative planning for the operation is the attention to achieving hemodynamic stability in the patient and the means to monitor such stability and to provide vigorous transfusion volume should it be necessary. For any major gastrointestinal bleed, the following resuscitative and patient care measures should be instituted as the first priority of care:
Transfer the patient to an ICU setting where continuous monitoring of vital signs is performed
Central line placement for both rapid fluid resuscitation and for monitoring volume status
Foley catheter to measure organ perfusion and hence resuscitation success
Availability of appropriate blood products should the bleeding worsen or continue unabated. These could include, as most appropriate, whole blood, fresh frozen plasma, packed red blood cells, and if significant transfusion requirements occur, platelets and cryoprecipitate
Reversal of any potential anticoagulant medication
Large bore intravenous access for transfusion requirements
Confirming the diagnosis of bleeding duodenal ulcer is normally done using flexible upper endoscopy. Usually endoscopic measures to control the bleeding are performed at the time of the procedure. Lack of efficacy of such measures is considered an appropriate indication to proceed with surgical intervention. Performing an extensive operation such as antrectomy, vagotomy, gastrojejunostomy, and oversewing of a bleeding duodenal ulcer is normally not performed without a clear diagnosis of bleeding duodenal ulcer. It is feasible that such a diagnosis can be inferred by the clinical picture but not confirmed endoscopically. In such situations, endoscopic success could have been limited by excessive blood in the lumen of the duodenum or due to other technical reasons. On occasion, diagnosis by angiography with inability to perform angiographic measures to stop the bleeding or failure of such measures could also serve as an appropriate confirmation of the diagnosis of bleeding duodenal ulcer and the need to perform surgical therapy.
Prior to surgery, a thorough history of the patient’s previous problems with gastrointestinal issues, including any history of previous ulcer disease or long-standing symptoms consistent with ulcer disease, is appropriate. Given such a history, the use of an
antrectomy with vagotomy, rather than just vagotomy and drainage procedure, for the treatment of complications of duodenal ulcer is more justified.
antrectomy with vagotomy, rather than just vagotomy and drainage procedure, for the treatment of complications of duodenal ulcer is more justified.
Surgical Procedure
The operation is, due to its nature as an emergency procedure for life-threatening bleeding, normally conducted as an open operation through an upper midline incision. Its performance as a laparoscopic operation could be feasible, but the two major factors that would make laparoscopy more difficult are the maintenance of hemodynamic stability in the setting of creating a pneumoperitoneum and the difficulty in suctioning the actively bleeding area in order to place the sutures properly to oversew the ulcer without losing the pneumoperitoneum and the operative field of vision.
Oversewing the Ulcer
Once an upper midline incision is made and the abdominal organs are made accessible, the first priority and hence also first step of the operation is to perform the oversewing of the ulcer. The steps of this portion of the operation are as follows:
The duodenum is exposed. A Kocher maneuver may assist in bringing the duodenum up into the field and should be used.
The pylorus is identified.
An anterior duodenal incision is made starting 1 cm beyond the pylorus, and extending 2 cm into the duodenum (Fig. 13.1).
The bleeding site should be within visualization using this access. On occasion, further extension of the duodenal end of the incision may be needed.
The bleeding ulcer is normally on the posterior surface of the duodenum, in the location of the gastroduodenal artery. The course of the artery is usually through the distal first part of the duodenum or most proximal second portion.
The ulcer bleeding vessel is now directly oversewn with three simple silk sutures. Other materials may be used, but the suture weight must be heavy enough to allow it to be tied to gather the ligated tissue together without breaking. A 2-0 weight suture is recommended.
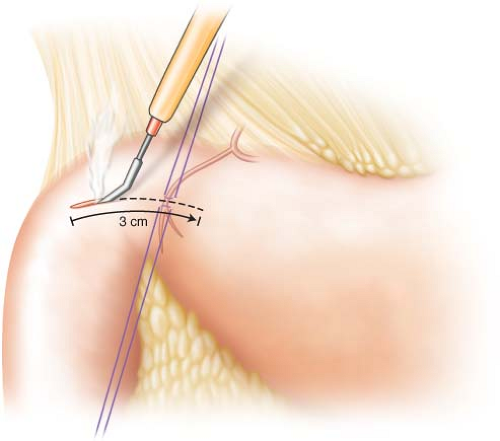
Figure 13.1 Performing an incision 1 cm distal to the pylorus and extending it 2 cm distally in the duodenum to expose the site of the bleeding ulcer.
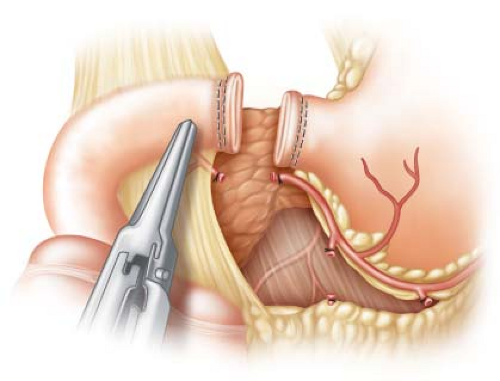
The sutures are placed as illustrated in Figure 13.2. One is at right angle to the course of the artery proximal to it, a second in that same orientation distal to it, and the third at a 90-degree orientation on the medial or proximal side of the bleeding to occlude the frequently present transverse pancreatic branch of the gastroduodenal artery.
Once the bleeding is controlled, the duodenotomy is closed with a running layer of absorbable suture.
Performing the Antrectomy
The antrectomy is now performed once it is confirmed that the most proximal duodenum is not excessively scarred and therefore is amenable to surgical closure. The steps of the antrectomy are as follows:
The plane underneath the surface of the most proximal duodenum is dissected to allow passage of a stapler through it. Small vessels in this area may need division with an ultrasonic scalpel.
The GIA-type stapler is fired across the most proximal duodenum at this location. The staple line should be beyond the pylorus. It should also be proximal to the closure of the duodenotomy whenever feasible (Fig. 13.3). Inclusion of the suture closure
of the duodenotomy will weaken that suture line, and if this occurs, the suture line must be reinforced to prevent disruption.
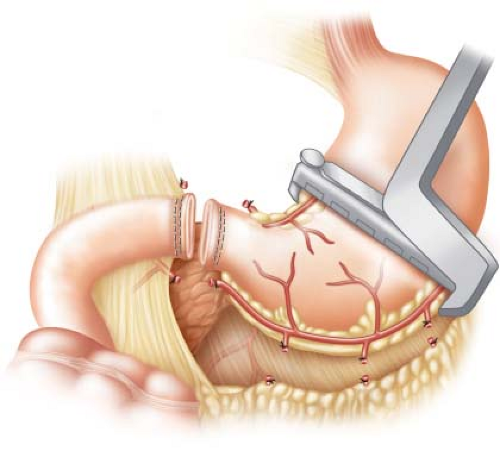
The site of proximal division of the stomach is determined. This is normally at the incisura on the lesser curvature of the stomach and in a point directly radially opposite to it on the greater curvature of the stomach. These sites are marked by local division of vessels adjacent to the lesser and greater curvatures of the stomach with the ultrasonic scalpel.
The vessels of the right gastroepiploic artery running adjacent to the greater curvature of the stomach along the antrum are divided using either suture ligation technique or with the ultrasonic scalpel. Special care is taken to ligate the main trunk of the right gastroepiploic artery.
The vessels along the lesser curvature of the stomach, beginning at the pyloric division, are also ligated in a similar fashion. Here the right gastric artery must be securely identified and ligated.
The stapler is used to divide the stomach at the previously determined sites of division (Fig. 13.4). Care must be taken to be sure no nasogastric or other tubes are in the lumen of the stomach. The blue, gold, or green load of the TA-type stapler is used, depending on the thickness of the gastric tissue.
Both the gastric staple line and the duodenal staple line are inspected for integrity and hemostasis. Simple sutures are used if any areas of concern are noted.
Performing Vagotomy
A truncal vagotomy is indicated in this setting. Optimal elimination of the cholinergic stimulation of gastric secretion is sought; hence complete or truncal vagotomy is performed. The steps of the vagotomy are as follows:
The phrenoesophageal ligament is divided anteriorly to expose the anterior surface of the esophagus. Dissection of the peritoneum is extended to the left to the angle of His and to the right to just past the right crus of the diaphragm.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree