Fig. 13.1
Lateral lymph nodes (yellow circles) defined by the Japanese Classification of Colorectal Carcinoma. Internal iliac nodes, common iliac nodes, obturator nodes and external iliac nodes constitute the lateral pelvic lymph nodes (white circles). (Red circles) are pericolic/perirectal lymph nodes along the colon and the rectum and (blue circles) are intermediate lymph nodes along the major vesseles (From Japanese Society for Cancer of the Colon and Rectum [9])
Rationale for Lateral Lymph Node Dissection
Lateral pelvic lymph node metastasis is found in about 15 % of cases of clinical stage II/III lower rectal cancer [12, 13]. Several studies from Japan have shown that the 5-year survival rate of patients with lateral pelvic lymph node metastasis is about 40 % [12–14], being comparable with that of patients with resectable liver or lung metastasis. Under the assumption that if lateral lymph node dissection not performed, local recurrence would develop in the form of metastasis to these nodes and become the cause of death, the estimated improvement in the 5-year survival rate would be 6 % (0.15 × 0.4 × 100), because 15 % of patients with lower rectal cancer have lateral pelvic lymph node metastasis and 40 % of those who undergo lateral lymph node dissection will survive for more than 5 years. These figures would indicate that lateral lymph node dissection should be considered whenever lateral pelvic lymph node metastasis is suspected preoperatively. This option is known as therapeutic lateral lymph node dissection. The Guidelines 2000 for Colon and Rectal Cancer Surgery also mention that in the context of clinically suspected lateral lymph node disease, dissection should be attempted in order to remove these nodes, if it is technically feasible [15].
Figure 13.2 shows representative CT images of lateral pelvic lymph node metastasis. However, in patients without lymph node enlargement, not all lateral pelvic lymph node metastases can be demonstrated by CT or MRI, and sometimes they are only revealed after lateral lymph node dissection. Because the diagnostic accuracy of CT or MRI for lateral pelvic lymph node metastasis is imperfect [16, 17], lateral lymph node dissection is also indicated in Japan even for patients without evident enlargement of such nodes. This option is known as prophylactic lateral lymph node dissection. However, even in Japan, the indications for prophylactic lateral lymph node dissection are controversial. Therefore, on behalf of the Japan Clinical Oncology Group (JCOG), a randomized controlled trial to confirm the efficacy of prophylactic lateral lymph node dissection is currently underway (the JCOG0212 trial) [18]. Because primary analysis of the trial results is planned for 2015, no survival data are yet available. In terms of morbidity and mortality, the rates of grade 3–4 postoperative complications were similar between mesorectal excision with lateral lymph node dissection and mesorectal excision alone. At the European Cancer Congress in 2013, urinary and sexual functions after this form of surgery were also reported to be similar in these two groups [19, 20]. A previous meta-analysis of extended lateral lymph node dissection had suggested that it was associated with an increased risk of urinary and sexual dysfunction, and did not confer any survival benefit [21]. This may have been due to the fact that previous retrospective studies of lateral lymph node dissection had included both autonomic nerve-preserving surgery and non-preserving surgery. In the JCOG0212 trial, however, autonomic nerve-preserving surgery was performed for all of the enrolled patients, thus accounting for the similarity of postoperative urinary and sexual functions between the groups. It is anticipated that the JCOG0212 trial will yield informative data for evaluation of prophylactic lateral lymph node dissection.
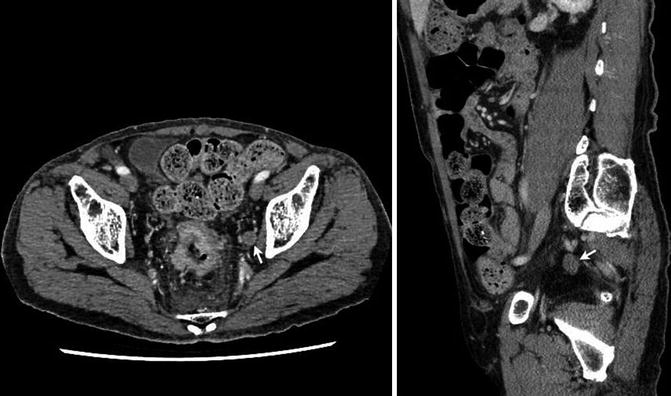
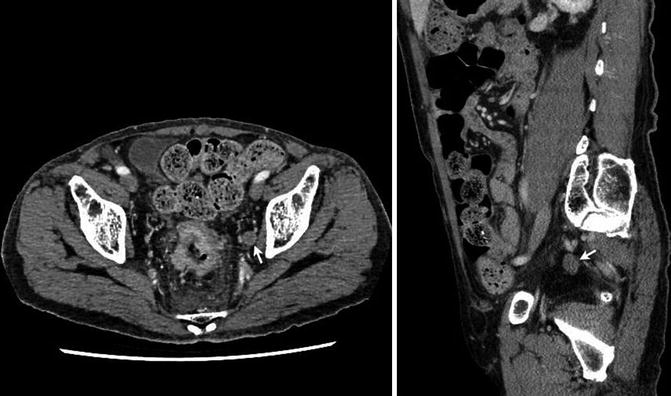
Fig. 13.2
Representative CT images (axial and sagittal sections) of lateral lymph node metastasis. Left latelaral pelvic lymph node enlargement is seen (arrows)
Indication Criteria for Lateral Lymph Node Dissection
The indication criteria for lateral lymph node dissection are stipulated in the 2010 Japanese Society for Cancer of the Colon and Rectum guidelines for the treatment of colorectal cancer [22]. Lateral lymph node dissection is indicated when the lower border of the tumor is located distal to the peritoneal reflection and has invaded beyond the muscularis propria (T3 or T4). This criterion is based on retrospective risk analysis of lateral pelvic lymph node metastasis [12]. The incidences of lateral pelvic lymph node metastasis in cases of clinical stage I rectal cancer and for tumors whose lower margin is located above the peritoneal reflection are very low. The lower border of the tumor is an important aspect of this criterion, because lateral lymphatic flow in the rectum exists below the peritoneal reflection. It is not appropriate to include the distance from the anal verge to the lower border of the tumor as part of the indication criteria, because the distance from the anal verge to the peritoneal reflection differs among individual patients.
Therapeutic and Prophylactic Lateral Lymph Node Dissection
As mentioned in the previous section, there are two types of procedure for lateral lymph node dissection: therapeutic and prophylactic. If a patient with rectal cancer has no clinical evidence of lateral pelvic lymph node metastasis, prophylactic dissection is indicated, whereas therapeutic dissection is indicated if such metastasis is present. Therapeutic and prophylactic dissection differ in their area of dissection and level of nerve preservation. In therapeutic dissection, the internal iliac nodes, common iliac nodes, obturator nodes and external iliac nodes are dissected, and the presacral and sacral promontory nodes are also dissected when metastasis is suspected. The autonomic nerves on the side where metastasis is suspected are resected. Therefore, if bilateral lymph node metastasis is suspected, the autonomic nerves are not preserved. In prophylactic dissection, the internal iliac nodes, common iliac nodes, obturator nodes and external iliac nodes are dissected, but the presacral and sacral promontory nodes are not. All of the autonomic nerves are preserved in principle.
The anatomy of the autonomic nervous system in the pelvis is an important point to consider for preservation of the autonomic nerves in rectal cancer surgery. Figure 13.3 shows the autonomic nerves after TME. Those in the pelvis include the superior hypogastric plexus, hypogastic nerve, pelvic (inferior hypogastric) plexus and pelvic splanchnic nerve. Identification of these autonomic nerves during surgery is very important for ensuring their preservation. Preservation procedures will be described in the next section.
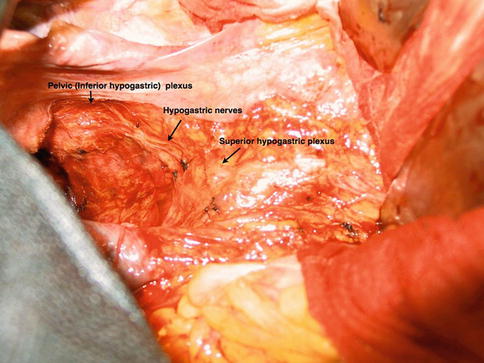
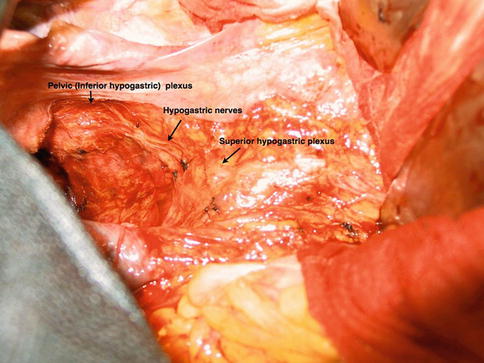
Fig. 13.3
Autonomic nerves in the pelvis. The superior hypogastric plexus, hypogastic nerve, and pelvic (inferior hypogastric) plexus can be identified
Procedure for Prophylactic Lateral Lymph Node Dissection
In this procedure, the internal iliac nodes, common iliac nodes, obturator nodes, and external iliac nodes are dissected and the autonomic nerves are preserved. During the dissection, if any lymph nodes with metastasis are confirmed, the dissection is converted to therapeutic lymph node dissection.
Confirmation of Autonomic Nerves
After mobilization of the sigmoid colon and upper rectum, the superior hypogastric plexus can be identified at the level of the aortic bifurcation (Fig. 13.4). The fibers extending from the superior hypogastric plexus to the right and left sides of the rectum are the hypogastric nerves. These are important landmarks for ensuring that the plane of dissection stays anterior and medial to the plexus and hypogastric nerves. If this plane is maintained, these nerves and the pelvic plexus can be preserved without difficulty. Recently, an ultrasonic scalpel (Harmonic Scalpel®) or an electrothermal bipolar tissue sealing system (Ligasure®) has been commonly used for lateral lymph node dissection, especially in laparoscopic surgery.
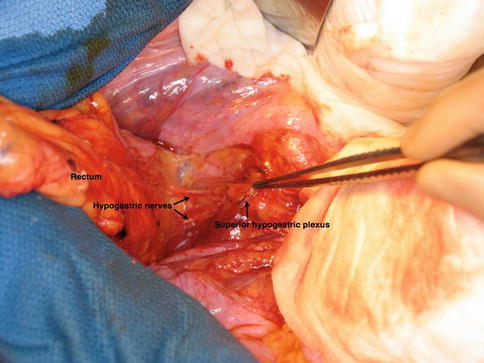
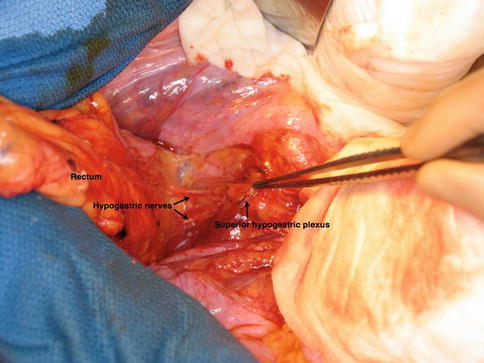
Fig. 13.4
Superior hypogastric plexus and hypogastric nerves. The superior hypogastric plexus has been picked up with forceps
Common and Proximal Internal Iliac Node Dissection
First, the ureters are exposed bilaterally, and then the ureters, the superior hypogastric plexus and the hypogastric nerves are lifted using retraction tapes to prevent accidental injury. The dissection begins along the inner side of the common and internal iliac vessels downward to the superior vesical artery while removing the fatty tissue covering the vessels. This fatty tissue includes the common and proximal internal iliac nodes. Within the layer just above the vessels, it is easy to dissect the fatty tissue and blood loss will be minimal. In prophylactic dissection, only the inner side of the common iliac vessels is dissected. After inner side resection, the fatty tissue along the outer side of the internal iliac artery is dissected. This area lies between the internal and external iliac vessels. Thereafter, dissection of the external iliac lymph nodes is performed.
External Iliac Lymph Node Dissection
The external iliac vessels are picked up using retraction tapes, and the fatty tissues only along the inner side of the vessels are dissected. After external iliac lymph node dissection, the internal obturator muscle is identified below and outside the external iliac vessels. This represents the lateral limit of lateral lymph node dissection.
Obturator Lymph Node Dissection
The obturator lymph nodes lie in the obturator fossa. At the center of the fossa, the obturator nerve runs in a cranial to caudal direction. Because the nerve is an important dissection landmark, it should be located before initiating lymph node dissection. The nerve is picked up using a retraction tape and the fatty tissues in the area are resected. The only major vessels are the obturator vessels in the fossa, and care should be taken to avoid them during the dissection to prevent bleeding. The distal limit of lateral lymph node dissection is the obturator membrane, and the dorsal limit is the piriformis muscle and sciatic nerves.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






