Chapter 27 Lateral Decubitus Approach to Minimally Invasive Low Anterior Resection
Preoperative evaluation, testing, and preparation
Patient positioning in the operating suite
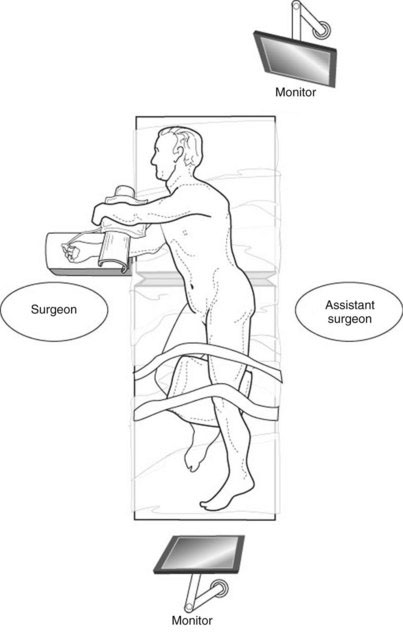
The patient is placed in the right lateral decubitus position (Fig. 27-1). The right leg is flexed 30 degrees at the hip, and the left leg is extended with a pillow placed between the knees. The buttocks are positioned toward the edge of the table. Sequential compression devices are placed on both legs, and the patient is taped securely to the table. The right arm is extended over an arm board, and the left arm is positioned over a pillow on a Mayo stand. An axillary roll is placed under the right axilla. The arms are properly cushioned and supported to avoid a perioperative neurapraxia. The table is flexed and the kidney rest may be raised, extending the left flank and maximizing the working space. The operative field is prepared and draped to allow exposure from the left nipple down to the pubic symphysis, and from the umbilicus to the posterior axillary line. The anus must be accessible under the drapes so as to place the EEA device, as if performing a colonoscopy. Two video monitors are required—one at the head of the table to the patient’s left, the other at the foot of the table.
Positioning and placement of trocars
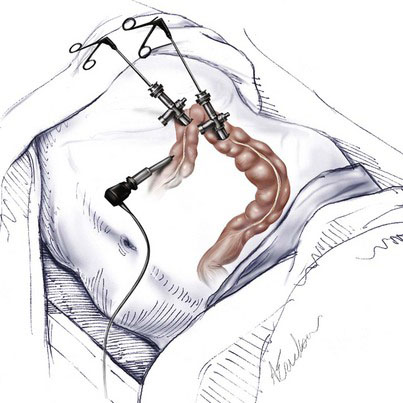
Laparoscopic low anterior and rectal resection in the right lateral decubitus position requires three trocars, with the option of a fourth (Fig. 27-2). A 10-mm trocar is inserted in the left midclavicular line, 2 to 3 cm above the level of the umbilicus. This serves as the optical port. A 5-mm trocar is inserted in the left subcostal region at the level of the anterior axillary line. This serves as the working port, through which the retraction and dissection instruments are placed. It can be converted to a 10-mm port if needed later in the operation. A 5-mm trocar is inserted under the left 11th rib at the level of the midaxillary line. This is used for the retraction and dissection instruments. If a fourth port is needed, it may be placed in the suprapubic region. A 10-mm 30-degree laparoscope is used for the procedure.
Operative technique
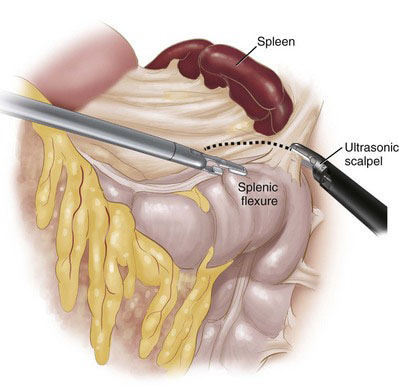
The advantage of the lateral decubitus approach becomes apparent during the dissection of the splenic flexure. As the colon is retracted inferiorly and medially with the right hand, the splenocolic ligament is transected (Fig. 27-3). This may best be performed using a sealing device because this ligament may contain small vessels. The flexure should fall away naturally from its attachments. The white line of Toldt then can be opened inferiorly toward the sigmoid colon. Careful attention to the planes of dissection must be maintained to avoid entering the lateral attachment of Gerota fascia, which would medialize the left kidney and reduce exposure of the operative field.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree