Laparoscopic Subtotal Gastrectomy and D1 Resection
Namir Katkhouda
Helen J. Sohn
John C. Lipham
Joerg Zehetner
Resectable gastric cancers involving the body and antrum are the main indication for subtotal gastrectomy with Roux-en-y gastrojejunostomy and regional lymphadenectomy (D1-resection: includes the perigastric lymph nodes stations 1–6 and the nodes along the left gastric artery station 7). A minimum of 5 cm proximal margin is required. Laparoscopic approach can be used when there are no contraindications for laparoscopy, such as multiple prior upper gastrointestinal operations, liver cirrhosis, poor cardiac status proven on stress test, pregnancy, or inability for the patient to give consent for laparoscopy.
Uncommon Indications
Benign tumors of the stomach such as gastrointestinal stromal tumor located in the proximal stomach that is too large for a wedge resection. No lymphadenectomy is required.
Complications of ulcer diseases such as bleeding and obstruction.
Gastroparesis with uncontrollable vomiting. Near total gastrectomy can be performed after all medical and other therapies have been exhausted. No lymphadenectomy is required.
Conversion of distal gastrectomy with gastroduodenostomy or loop gastrojejunostomy.
Contraindications for subtotal gastrectomy are cancers of the proximal stomach or diffuse gastric cancer both of which will necessitate a total gastrectomy for an R0 resection with disease-free microscopic margins. Metastatic cancers are treated by chemotherapy unless bleeding, obstruction, or perforation is present. Bleeding or perforated gastric cancers should be treated with a resection and obstructed cancers can be treated by either a resection or a bypass. Invasion of adjacent organs such as colon, liver, or spleen is not a contraindication to resection.
Upper endoscopy is performed to assess the location and the extent of the disease.
Endoscopic ultrasound is performed to assess the lymph nodes in the celiac axis and obtain a fine needle biopsy for staging and planning treatment.
CT scan of the chest, abdomen, and pelvis is important to assess the presence of metastasis in distant lymph nodes, peritoneum as studding and ascites, or distant organs.
PET scan is used to further assess for metastatic diseases. There may be limited usefulness if the primary tumor does not show increased uptake of the tracer.
Standard cardiopulmonary workup should be done to assess operability of the patient.
Laparoscopic surgery should be performed using the same principle as open surgery.
Positioning
Patient is supine in low lithotomy position to allow the surgeon to stand between the legs. Both arms should be tucked to allow placement of retractor posts onto the bed at the nipple level. Patient is placed in steep reverse Trendelenburg position to expose the upper abdominal structures with gravity. This is the ideal position for all upper gastrointestinal operations, and the surgeon faces the screen above the head of the patient. The first assistant is to the right and the camera assistant to the left of the patient. This enables the surgeon to have a straight view of the relevant screen. A Mayo stand for the surgeon’s instruments is usually placed to the surgeon’s right and the scrub technician stands to the left. It is important in this position for advanced upper abdominal procedures to avoid deep venous thrombosis by using bilateral lower extremity sequential compression devices and comfortably padding the knees, ankles, and legs.
Port Placement
Before starting the operation it is important to insert a nasogastric tube to decompress the stomach, thus avoiding any injury to the stomach upon insertion of the Veress needle.
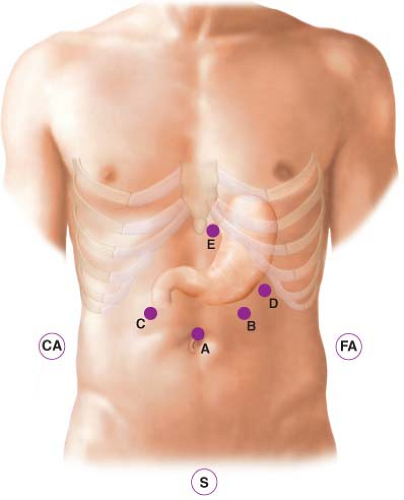
The first 12-mm trocar is introduced after the creation of the pneumoperitoneum with the Veress needle using an optical port in the midline superior of the umbilicus (Fig. 16.1). The reason for midline rather than left paramedian for this port is to extend this incision later in the procedure for specimen removal and introduction of the circular stapler if used. This small incision can also be used for jejunojejunostomy and optional feeding jejunostomy tube placement. This port is used for the camera.
A second 12-mm trocar is placed in the left subcostal position in the midclavicular line as a primary working port.
Three additional 5 mm or 10 mm trocars are used:
One in the subxyphoid position used to make a subcutaneous tract for the introduction of the Nathanson Hook Liver Retractor (Automated Medical Products Corporation, Sewaren, NJ). This retractor is secured to the right bed post using an Iron Intern (Automated Medical Products Corporation, Sewaren, NJ).
Two retracting ports are placed in the right and left subcostal margins.
Technique
We will describe two common techniques:
Greater Curvature First Technique
Before the actual dissection starts, it is important to check on the various landmarks: the curvatures of the stomach, the gastrocolic ligament and the gastroepiploic arcade, the inferior aspect of the antrum, the duodenum, the pyloric muscle, the lesser sac, and the right gastric artery. The limit of the antrum and the proposed site of the gastrojejunostomy is marked using electrocautery. The assistant begins the procedure by retracting the greater curvature of the stomach using the lateral port. The surgeon uses a grasper and the ultrasonic shears to create windows in the gastrocolic ligament (Fig. 16.2




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree