Laparoscopic Sigmoid Colectomy
KEY STEPS
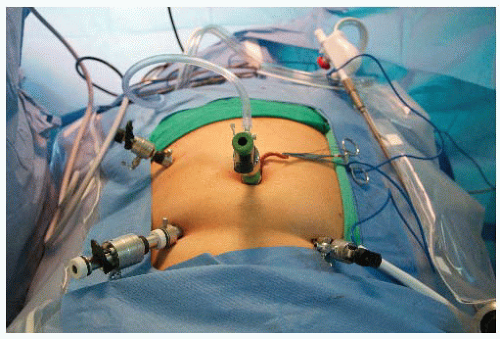
1. Insertion of ports: 10-mm umbilical Hasson technique; 12-mm right iliac fossa; 5-mm right upper quadrant; 5-mm left iliac fossa.
2. Patient rotated to the right and steep Trendelenburg.
3. Laparoscopic assessment and the small bowel and omentum moved toward right and upper quadrants.
4. Inferior mesenteric pedicle defined and divided, protecting the ureter and presacral autonomic nerves.
5. Retroperitoneal mobilization of the descending colon mesentery.
6. Division of lateral attachments of the sigmoid and descending colon to splenic flexure, and flexure mobilization as required.
7. Mobilization of the rectosigmoid junction and the area for transection chosen.
8. Transection of the upper rectum and mesorectum.
9. Exteriorization and resection of the sigmoid colon through left lower quadrant incision.
10. Reinsufflation and anastomosis.
11. Port closure.
ADDITIONAL ADVICE
1. If it is difficult to find the presacral space on the right side of the mesentery, consider changing to a lateral mobilization of the sigmoid before risking nerve or other injury.
2. Making a long incision in the peritoneum to mobilize a long segment of inferior mesenteric artery (IMA) facilitates safe identification of the presacral space and protection of nerves and ureter.
3. It is often easier to enter the presacral space just inferior to the sacral promontory, and then work back toward the origin of the inferior mesenteric artery.
4. Once the inferior mesenteric artery and vein are divided, mobilize as much of the descending mesocolon as possible from the medial approach, to facilitate later lateral dissection.
5. When performing the lateral mobilization of the sigmoid colon, draw the colon medially and anteriorly to display the space behind the sigmoid and its mesentery, which has already been mobilized with the medial dissection.
6. If it appears necessary to dissect up to the splenic flexure, mobilize it and any mesentery necessary at this stage, to avoid potentially compromising blood flow after exteriorizing the specimen, as it is difficult to assess blood flow once the bowel has been returned to the abdomen with the anvil in place.
7. Be careful to divide at the rectosigmoid junction or the chosen transection point with stapler cartridges carefully placed perpendicularly to the axis of the bowel.
8. When placed across the sacral promontory and into the pelvis, the proximal colon—with stapler anvil in situ—should lie easily in the pelvis while the patient is in Trendelenburg position, demonstrating a likely tension-free anastomosis.
PATIENT POSITIONING
The patient is placed supine on the operating room (OR) table on a bean bag. After induction of general anesthesia and insertion of an oral gastric tube and a Foley catheter, the legs are placed in yellow fin stirrups. The arms are tucked at the patient’s side and the bean bag is aspirated. The left arm is left out if the patient is too obese to get both arms on the OR table. The abdomen is prepared with antiseptic solution and draped routinely.
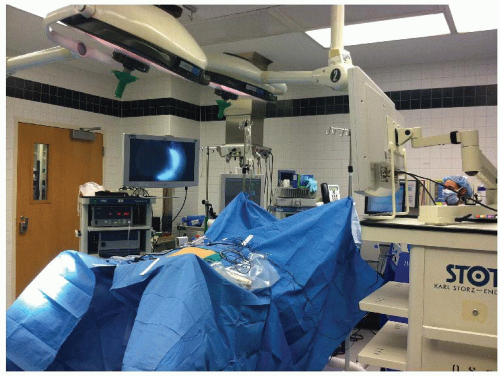
INSTRUMENT POSITIONING
The primary monitor is placed on the left side of the patient, at approximately the level of the hip. The secondary monitor is placed on the right side of the patient at the shoulder level and is primarily for the assistant during the early phase of the operation and port insertion (see Fig. 15.1). The operating nurse’s instrument table is placed between the patient’s legs. There should be sufficient space to allow the operator to move from either side of the patient to between the patient’s legs if necessary. The primary operating surgeon stands on the right side of the patient at the level of the patient’s hip, with the assistant standing on the patient’s left. The assistant moves to the right side at the level of the patient’s shoulder once ports have been inserted. If a second assistant is available, he/she stays on the patient’s left side. A 0-degree camera lens is used.
UMBILICAL PORT INSERTION
This is performed using a modified Hassan approach. A vertical 1-cm subumbilical incision is made. This is deepened down to the linea alba, which is then grasped on each side of the midline using Kocher clamps. Cautery is used to open the fascia between the Kocher clamps and Kelly forceps are used to open the peritoneum bluntly. It is important to keep this opening small (1 cm) to minimize air leaks. Having confirmed entry into the peritoneal cavity, a purse string of 0 polyglycolic acid is sutured around the subumbilical fascial defect (umbilical port site) and a Rommel tourniquet applied. A 10-mm reusable port is inserted through this port site allowing the abdomen to be insufflated with CO2 to a pressure of 12 to 15 mmHg.
LAPAROSCOPY AND INSERTION OF REMAINING PORTS
The camera is inserted into the abdomen and an initial laparoscopy is performed carefully evaluating the liver, small bowel, and peritoneal surfaces. A 12-mm port is inserted in the right lower quadrant, approximately 2 to 3 cm medial and superior to the anterior superior iliac spine. This is carefully inserted lateral to the inferior epigastric vessels, paying attention to keep the tract of the port going as perpendicular
as possible through the abdominal wall. A 5-mm port is then inserted in the right upper quadrant at least a hand’s breath superior to the lower quadrant port. A 5-mm left lower quadrant port is usually inserted. Rarely, in the case of a difficult splenic flexure, a 5-mm left upper quadrant port may also need to be inserted. Again, all of these remaining ports are kept lateral to the epigastric vessels (Fig. 15.2).
as possible through the abdominal wall. A 5-mm port is then inserted in the right upper quadrant at least a hand’s breath superior to the lower quadrant port. A 5-mm left lower quadrant port is usually inserted. Rarely, in the case of a difficult splenic flexure, a 5-mm left upper quadrant port may also need to be inserted. Again, all of these remaining ports are kept lateral to the epigastric vessels (Fig. 15.2).
DEFINITIVE LAPAROSCOPIC SETUP
The assistant now moves to the patient’s right side, standing at shoulder level. The patient is rotated with the left side up and right side down, to approximately 15 to 20 degrees tilt, and often as far as the table can go. This helps to move the small bowel over to the right side of the abdomen. The patient is then placed in the steep Trendelenburg position. This again helps gravitational migration of the small bowel away from the operative field. The surgeon then inserts two atraumatic bowel clamps through the two right-sided abdominal ports. The greater omentum is reflected over the transverse colon so that it comes to lie on the stomach (Fig. 15.3). If there is no space in the upper part of the abdomen, one must confirm that the orogastric tube is adequately decompressing the stomach of gas. The small bowel is moved to the patient’s right upper quadrant, allowing visualization of the inferior mesenteric pedicle. This may necessitate the use of the assistant’s 5-mm atraumatic bowel clamp through a left lower quadrant port in order to adequately tent up the sigmoid mesentery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree