Chapter 10 Laparoscopic Roux-en-Y Gastric Bypass with Medial Rotation of the Left Hepatic Lobe
Preoperative assessment and preparation
A multidisciplinary approach is necessary for preoperative evaluation and optimization of the bariatric patient. A dedicated team of internists, cardiologists, pulmonologists, gastroenterologists, nutritionists, and psychologists is used in the preoperative evaluation and preparation of the bariatric patient for surgery (Table 10-1). Any medically reversible causes of obesity such as hypothyroidism are investigated and treated. A careful history of all medications is obtained, including over-the-counter and herbal supplements.
Table 10-1 Preoperative Assessment Team
| Psychologist | Mental health assessment |
| Nutritionist | Low-calorie diet program |
| Physical therapist | Exercise program |
| Internist | Complete blood count, metabolic panel, liver function tests, iron studies, prostate-specific antigen level for males >50 years old |
| Endocrinologist | Thyroid function tests, parathyroid hormone, vitamins A, D, B12 levels |
| Gastroenterologist | Upper endoscopy, colonoscopy for patients >50 years old |
| Pulmonologist | Pulmonary function test, sleep apnea study |
| Cardiologist | Echocardiogram, stress test |
| Radiologist | Gallbladder sonogram, venous duplex, inferior vena cava filter for high-risk patients, mammogram for women >40 years old |
| Gynecologist | Papanicolaou test for women >35 years old |
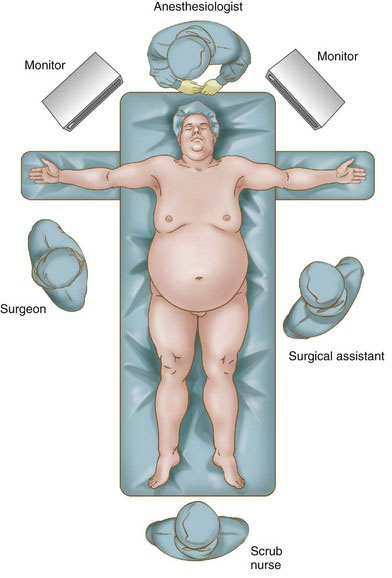
Patient positioning
The patients are placed supine on the operating room table with both arms extended (Fig. 10-1). The Lloyd-Davies position can also be employed, with the surgeon standing between the legs. However, we feel the supine position with the surgeon at the patient’s right side reduces stress on the patient’s legs. A Foley catheter is not routinely placed, and patients are asked to void just before entering the operating room. Before induction of anesthesia, they are given a dose of broad-spectrum antibiotics, and intermittent pneumatic compression devices are placed on both legs. A foot board is placed, but with the authors’ technique, we have never required the use of a steep reverse Trendelenburg position. The bariatric anesthesiologists routinely employ a fiberoptic laryngoscope that greatly facilitates endotracheal intubation.
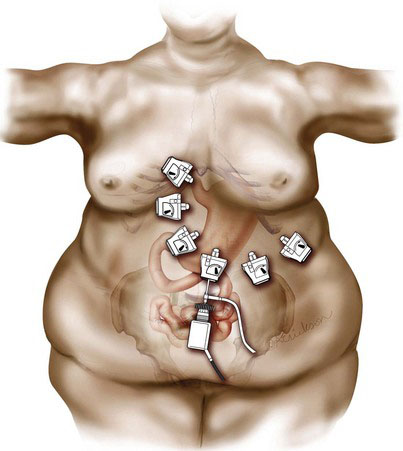
Placement of trocars
The authors’ choice of access is the Veress needle, which is usually placed at the umbilicus, unless there is a hernia or a concern for adhesions. In these cases, we place it either at the Palmer point or at the site of the first trocar. An open technique is rarely used. Once pneumoperitoneum is established, a 10-mm trocar is placed 16 to 18 cm below the angle of His. The surgeon calculates this location by placing the base of the palm just above the left costal margin and making the incision at the tip of the third finger. A 10-mm 30-degree laparoscope is placed through this trocar, and the Veress needle and its trajectory are visualized to ensure that there has been no injury on insertion. The needle is removed under direct visualization, and the insufflator is connected to the trocar. A 5-mm trocar is inserted just below and to the right of the xiphoid process. This trocar is angled toward the patient’s left shoulder so that it comes through the falciform. Through this trocar, the left lobe of the liver is retracted anteriorly and cephalad, making it possible to visualize the angle of His and determine the approach. Once this is done, the remaining trocars are triangulated around the angle of His, as illustrated in Fig. 10-2.
Operative technique
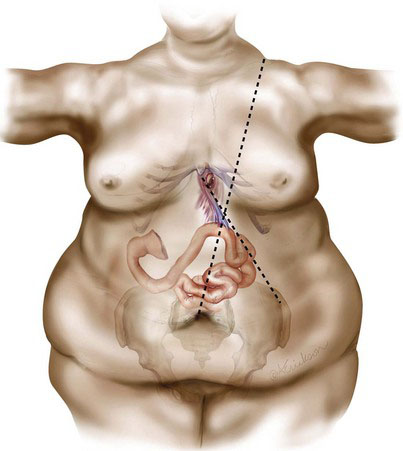
Creating the Biliopancreatic Limb
The greater omentum is swept cephalad to reveal the transverse mesocolon, which is retracted superiorly by the assistant with atraumatic graspers. The ligament of Treitz is then identified, keeping in mind its relatively constant anatomic location at the intersection between lines drawn from the left shoulder to the umbilicus and the xiphoid to the left anterior-superior iliac spine (Fig. 10-3).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree