Chapter 7 Laparoscopic Revision of Failed Fundoplication and Hiatal Hernia
Operative indications
Anatomic Failure
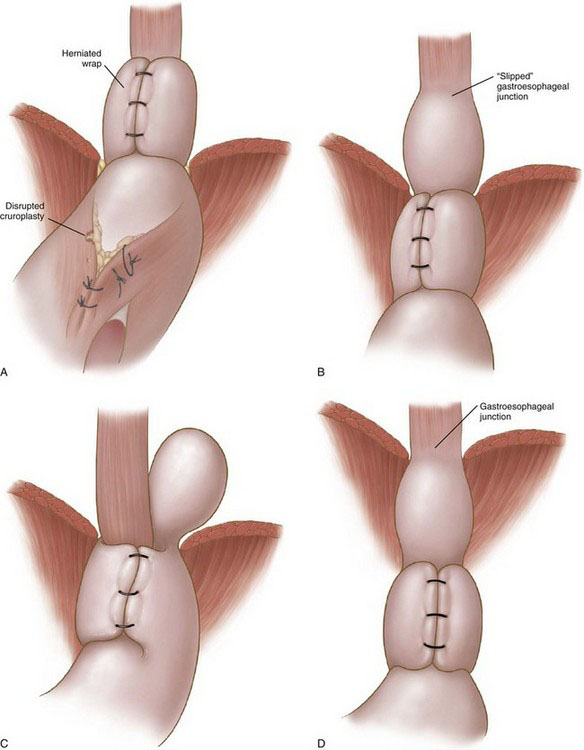
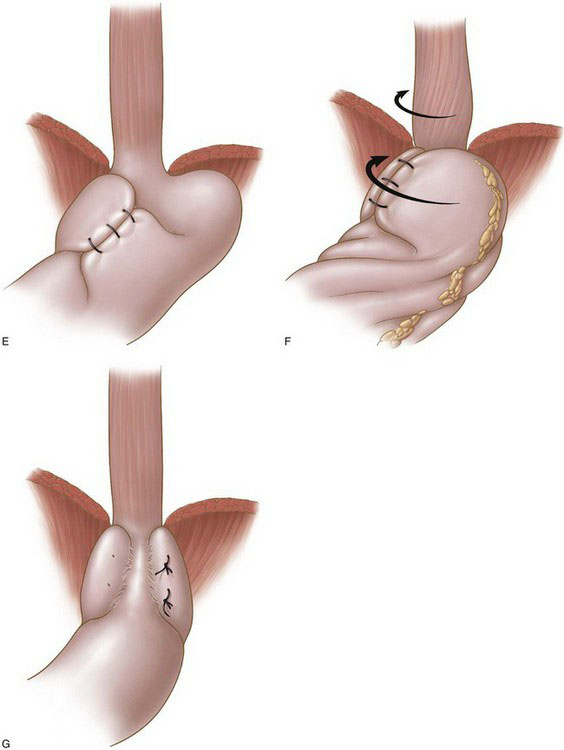
Seven types of anatomic failure may be encountered.
• Wrap migration (44%). A portion of the wrap or the entire wrap has migrated into the mediastinum (Fig. 7-1A). The proposed etiologic factor is inadequate crural closure owing to poor technique or weak tissue, or both; disruption of the cruroplasty results in migration of the wrap into the mediastinum.
• Slipped hernia (16%). The gastroesophageal junction has slipped into the mediastinum, whereas the wrap remains below the diaphragm (Fig. 7-1B). It has been postulated to result from the presence of a short esophagus or inadequate mobilization of the esophagus during the primary procedure. The latter is a more probable mechanism.
• Paraesophageal hernia (16%). Both the body of the wrap and the gastroesophageal junction remain below the diaphragm, whereas a part of the stomach has migrated into the mediastinum, posterior to the esophagus (Fig. 7-1C). This type of failure is a result of the combination of a loose wrap and a poor crural closure, which allows part of the posterior portion of the wrap to migrate into the mediastinum.
• Displaced wrap (10%). The wrap has slipped caudad on the body of the stomach, resulting in formation of a fundal pouch (Fig. 7-1D). The reasons for this type of failure are elusive; inadequate anchorage of the fundoplication may play a role. Retention of food in the herniated pouch may result in an increase of its size and further caudad slippage of the wrap (hourglass stomach).
• Misplaced wrap (4%). The plication has been constructed by the fundus and the body of the stomach because of misidentification of the anatomy at the initial operation (Fig. 7-1E).
• Twisted wrap (6%). Torsion of the wrap is thought to result from insufficient division of the short gastric vessels and continuous traction counterclockwise (Fig. 7-1F).
• Disrupted wrap (4%). A part of the fundoplication or the entire fundoplication has been disrupted. Inadequate construction of the fundoplication (superficially placed sutures) may account for this failure (Fig. 7-1G).
Preoperative evaluation, testing, and preparation
Computed Tomography and Ultrasonography
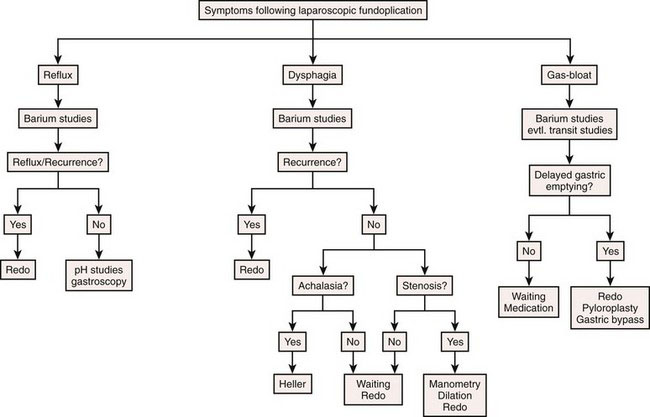
A diagnostic algorithm based on clinical history, patient complaints, symptom frequency, and severity is essential for the selection of suitable candidates for operative treatment and is presented in Figure 7-2.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree