Laparoscopic Resection Rectopexy
KEY STEPS
1. Insertion of ports: 10-mm umbilical open technique; 12-mm right iliac fossa; 5-mm right upper quadrant; 5-mm left iliac fossa.
2. Patient rotated to the right and slight Trendelenburg position.
3. Laparoscopic assessment and the small bowel and omentum moved toward the right upper quadrant.
4. Inferior mesenteric artery pedicle identified from medial aspect and elevated off the retroperitoneum. Left ureter identified and the inferior mesenteric artery divided distal to take off of left colic artery.
5. Medial-to-lateral mobilization of the sigmoid colon with little dissection of the descending colon.
6. Lateral mobilization of the sigmoid colon but limited mobilization of the left colon.
7. Rectal mobilization. Dissection behind the posterior 60% of the rectum in the presacral plane.
8. Mesorectal mobilization of the lateral aspects of the rectum until the prolapse is fully reduced.
9. Rectum stapled proximally in upper third, peritonealized segment, at a level which assures anastomosis just rostral to sacral promontory.
10. Extracorporeal resection of descending colon-sigmoid colon junction via muscle-splitting incision at left lower quadrant (LLQ) trocar site.
11. Closure of LLQ wound and intracorporeal circular stapled colorectal anastomosis under laparoscopic guidance.
12. Traction on the rectum out of the pelvis under appropriate tension and sutured rectopexy of both sides of the mesorectum (distal to the anastomosis) to the sacral promontory using a permanent suture.
13. Closure of ports greater than 5 mm in size.
ADDITIONAL ADVICE
1. During the rectal mobilization, observe the mesorectal plane.
2. Rectal dissection should usually be limited to the posterior wall, but the lateral attachments and even anterior rectum may require mobilization for a distal prolapse.
3. The lower lateral attachments (lateral stalks) should generally be preserved; the exception is when further dissection is needed to completely reduce a very distal prolapsing segment.
PATIENT POSITIONING
The patient is placed supine on the operating table on a bean bag. After induction of general anesthesia and insertion of an orogastric tube and a Foley catheter, the patient’s legs are placed in yellow fin stirrups. The arms are tucked at the patient’s side and the bean bag is aspirated. The abdomen is prepared with antiseptic solution and draped routinely (Chapter 2).
INSTRUMENT POSITIONING
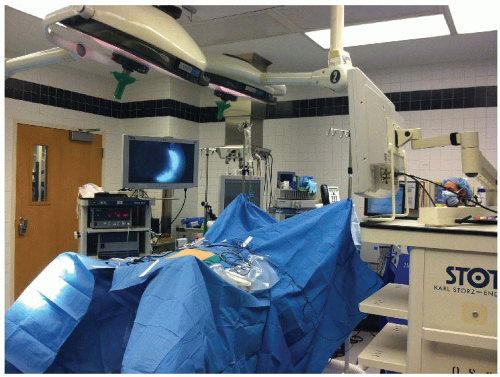
The primary monitor is placed on the left side of the patient at approximately the level of the hip. The secondary monitor is placed on the right side of the patient at the same level and is primarily for the assistant during port insertion and the early phase of the operation (see Fig. 24.1). The operating nurse’s instrument table is placed between the patient’s legs. There should be sufficient space to allow the operator to move from either side of the patient to between the patient’s legs if necessary. The primary operating surgeon stands on the right side of the patient with the assistant standing on the patient’s left, and moving to the right side, standing toward the head of the patient to the surgeon, once ports have been inserted. A 0-degree camera lens is used.
UMBILICAL PORT INSERTION
This is performed using a modified Hasson approach (Chapter 3). A vertical 1-cm subumbilical incision is made. This is deepened down to the linea alba, which is then grasped on each side of the midline using Kocher clamps. A scalpel (no. 15 blade) is used to open the fascia between the Kocher clamps and Kelly forceps are used to open the peritoneum bluntly. It is important to keep this opening small (<1 cm) to
minimize air leaks. Having confirmed entry into the peritoneal cavity, a purse string of 0 polyglycolic acid is sutured around the subumbilical fascial defect (umbilical port site) and a Rommel tourniquet is applied. A 10-mm reusable port is inserted through this port site allowing the abdomen to be insufflated with CO2 to a pressure of 12 mmHg.
minimize air leaks. Having confirmed entry into the peritoneal cavity, a purse string of 0 polyglycolic acid is sutured around the subumbilical fascial defect (umbilical port site) and a Rommel tourniquet is applied. A 10-mm reusable port is inserted through this port site allowing the abdomen to be insufflated with CO2 to a pressure of 12 mmHg.
LAPAROSCOPY AND INSERTION OF REMAINING PORTS
The camera is inserted into the abdomen and an initial laparoscopy is performed carefully evaluating the liver, small bowel, and peritoneal surfaces. A 5-mm port is inserted in the right lower quadrant approximately 5 cm medial and superior to the anterior superior iliac spine. This is carefully inserted lateral to the inferior epigastric vessels, paying attention to keep the tract of the port going as perpendicular as possible through the abdominal wall. A 5-mm port is then inserted in the right upper quadrant at least a hand’s breadth superior to the lower quadrant port. A left lower quadrant (LLQ) 5-mm port is inserted. Again all of these remaining ports are kept lateral to the epigastric vessels.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree