Chapter 12 Laparoscopic Repair of Perforated Peptic Ulcer
Patient positioning
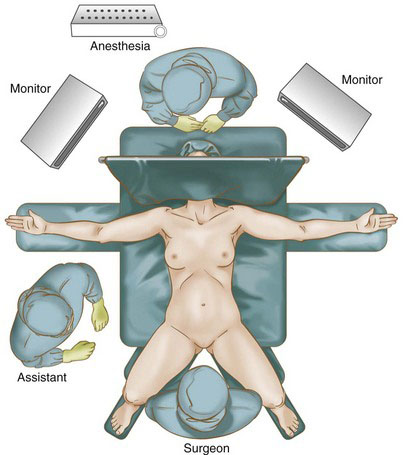
The patient is placed in the modified lithotomy (Lloyd-Davies) position. The surgeon stands between the patient’s legs and the assistant on patient’s right side, with the monitors positioned on either side of the head of the table (Fig. 12-1). Care is taken to ensure that all pressure points are adequately padded.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree