Fig. 12.1
(a) Bilateral interfascial nerve-sparing technique has been performed. The prostate has been removed and the neurovascular bundles have not been excised (white arrows). The lateral endopelvic fascia is incised bilaterally. The next step of the procedure is the performance of the vesicourethral anastomosis. (b) Bilateral intrafascial nerve preservation of the neurovascular bundles has been performed (yellow arrows). During the intrafascial approach the lateral endopelvic fascia is not incised. The puboprostatic ligaments have been preserved (yellow circles). The puboprostatic ligaments represent a landmark for the intrafascial approach as the dissection of the periprostatic fascias is initiated over the prostate at the reflection of the puboprostatic ligaments
The surgical steps of the procedure are almost identical, with minor modifications amongst the investigators with exception of the extraperitoneal or transperitoneal access [6–8, 21]. The patient is in Trendelenburg position and five trocars are usually placed (three 5 mm, two 12 mm). A 12 mm trocar is inserted in the umbilicus for the insertion of the optics. Another 12 mm trocar is positioned approximately two fingers-breadths medial to the left anterior superior iliac spine. A 5 mm trocar is inserted two fingers-breadths medial to the left of the midline, two-thirds of the way between the pubis and the umbilicus. Another 5 mm trocar is positioned in the right pararectal line cranially and one more is inserted medial to the right anterior superior iliac spine. Balloon dissection under direct visualization and insufflation of the preperitoneal space for the creation of the operative field follows in the case of the extraperitoneal approach.
In the transperitoneal approach, dissection of the lower peritoneum takes place without any balloon dilation and access to the prostate is achieved. Minor differences in the sequence of the steps of the procedure have been described by various investigators [20, 21]. The Intrafascial nerve-sparing EERPE is presented as a technical example [14].
An incision is made bilaterally in the periprostatic fascia at the reflection of the puboprostatic ligaments over the prostate and the plane between the prostate and fascias is developed. The latter plane allows the gradual detachment of the prostate from the fasciae surrounding the organ. Dissection of the bladder neck is then performed with careful mobilization of the branches of the NVBs while incising the dorsal bladder neck. The dissection is then continued dorsally and the seminal vesicles are mobilized with sharp and blunt dissection. The Denonviller’s fascia is detached from the prostate by blunt dissection strictly in the midline with the direction of the dissection towards the apex of the prostate. Blunt dissection takes place for the detachment of the prostatic pedicles from the surrounding fascias while clipping and careful cutting of the prostatic pedicles is performed. Ligation of the Santorini’s plexus by Vicryl 2-0 suture follows. The prostate is transected sharply from the external sphincter and the urethra. The vesicourethral anastomosis is performed with usually by nine interrupted sutures and the specimen is extracted for the accomplishment of the procedure.
Regarding nerve-sparing technique, energy-free dissection is utilized in order to preserve as much nerve fibers of the NVBs as possible. Although, the extent of anatomic dissection remains under investigation, intrafascial dissection is associated with improved post-operative potency in comparison to the interfascial approach [13, 14, 22].
12.3 Functional Results
Continence
Postoperative continence rates were high since the introduction of LRP [23]. In fact, the first reports on the outcome of the technique included data from large series of patients and showed continence rates between 75 and 80 % over a 6-months follow-up period [24, 25]. Large prospective studies have reported continence rates even greater than 93 % [26, 27]. Olsson et al. studied a large population by the use of validated questionnaires for a period of 12 months. At 6 months, none of the patients used more than one pad daily while 56.8 % of the patients reported no leakage at all [28]. The EPIC questionnaire was used by Link et al. for the assessment of postoperative continence and observed that 93.4 % of the patients were continent at 12 months follow-up [29]. Rassweiler et al. have reported continence rates of 33 % for their series at discharge from the hospital and 97 % after 12 months. The steep learning curve of the procedure seems to be an obstacle for centers that are not specialized in laparoscopy [30]. Other investigators confirmed the positive results with continence rates up to 97 % and follow-up periods up to 2 years [4, 31].
EERPE has offered comparable results to those of LRP [6, 13, 32]. A study by Stolzenburg et al. including 2,400 patients showed that 71.7 % of the patients were continent at 3 months after surgery and 94.7 % were continent at 12 months [6]. The intrafascial EERPE demonstrated even more promising results with a continence rate of 72.7 % at 3 months postoperatively, 85.3 % at 6 months, and 94.3 % at 12 months [13]. Similar experience with the extraperitoneal approach was presented by Rozet et al. [33]. The authors reported continence in 84 % of the patients and only 7 % of them using one-pad daily during the first year of follow-up.
Conflicting data are currently available regarding possible factors that influence postoperative continence. Several refinements of the LRP and EERPE have been proposed in an attempt to accelerate the postoperative recovery of continence.
Milhoua et al. suggested that large prostate size could be associated with a delay in recovery of post-operative continence [34]. In addition, factors related to the prostate cancer have not been recognized to predict post-operative continence [35]. Previous surgery of the prostate does not seem to significantly influence the postoperative continence. Menard et al. and Stolzenburg et al. reported high continence rates in patients that had previously undergone Transurethral Resection of the Prostate (TURP) and the results are based on long follow-up periods up to 2 years [36, 37]. Nevertheless, careful dissection of the urethra from the prostate and insertion of ureteral stents for the visualization of the ureteral orifices intraoperatively are advised during the performance of LRP/EERPE in the above patient population.
Careful bladder neck preservation has been proven to provide additional benefit in early postoperative continence without any influence on positive surgical margin (PSM) rates in several comparative studies [18, 19, 38]. Thus, the bladder neck stump after the dissection of the prostate from the bladder should remain as narrow as possible in order to allow faster recovery of continence. NVB preservation may be associated with faster recovery of continence [13, 39]. Posterior musculofascial reconstruction has also been proposed to have an impact in the faster recovery of postoperative continence. In fact, a recent systematic review reported an improvement of continence rates in the first 30 days after surgery, PSMs are similar to the patients without reconstruction and complication rates remain controversial [17]. Excellent long-term results on continence have been reported by several investigators. It should be noted that a significant improvement in continence rates is not expected beyond the first 12 months [40, 41].
Erectile Function and Potency
The quality of life of patients that have undergone radical prostatectomy is significantly influenced by the preservation of erectile function and potency (erections sufficient for intercourse). The recovery of potency and the time in which it occurs after LRP is related to the age and pre-operative potency of the patient. The performance of nerve-sparing technique is a predominant factor for the recovery of potency [29]. In addition, the preservation of accessory pundendal artery has also got a favorable impact on the recovery of potency and should be considered in patients that have the latter anatomical structure [42, 43].
The first experience with the preservation of the prostatic NVBs demonstrated improved potency rates in comparison to conventional technique. Although potency after non-nerve-sparing LRP was observed in 41 % of the cases, unilateral and bilateral nerve-sparing resulted in potency rates of 44 and 53 %, respectively [44]. Moreover, Roumeguere et al. showed that more spontaneous erections were present in patients who underwent LRP in comparison to those of the open approach [45].
Patients younger than 60 years of age have been reported to have potency rates ranging between 61 and 78.6 % over a 2-year follow up period [26, 32]. In the extraperitoneal approach, overall potency rates of 44 and 72 % were reported for unilateral and bilateral NVB preservation in a 12-month follow-up period. Higher rates of potency were observed in younger patients (below 55 years of age) with the respective figures to be 50 and 84.9 % [6].
The intrafascial approach is based on recent anatomical data that document the presence of a wide nerve fiber distribution in the fascias surrounding the prostate. Thus, a more extensive preservation of the NVBs and the surrounding prostatic fascias has been proposed with the introduction of the intrafascial nerve-sparing approach [13]. A significant benefit in postoperative continence has been documented in 200 patients undergoing intrafascial EERPE in comparison to those undergoing interfascial (conventional NVB preservation) [22]. Potency rates in patients who underwent bilateral intrafascial nerve-sparing technique were 93.5 % (for patients <55 years old), 83.3 % (for patients 55–65 years old), and 60 % (for patients >65 years old) at 12 months. The respective potency figures for the bilateral interfascial group were 77.1, 50, and 40 %. The overall potency rates are also favorable for the intrafascial approach: 82.8 % versus 64.8 % for the interfascial group. Other investigators reported rates up to 97 % in patients treated by intrafascial nerve-sparing after 1-year [46]. Nevertheless, the above results were not confirmed by other investigators [47]. It is important to note that the oncological outcome does not seem to be compromised by the intrafascial dissection [13, 47]. The use of athermal, energy-free technique during a nerve-sparing LRP/EERPE has been suggested by several investigators since the use of ultrasonic scissors or bipolar coagulation at the site of NVBs has a documented disadvantage in postoperative potency (Fig. 12.2a, b) [48]. The preservation of seminal vesicles has been also proposed by Shah et al. to have a favorable impact to potency. Nevertheless, additional studies are necessary for the extraction of solid results regarding this technique [49]. Long-term results on potency showed a slight but not significant improvement of potency at 24 months [40].
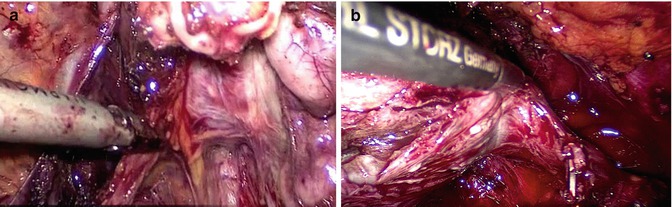
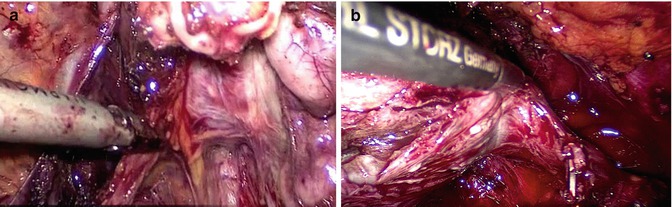
Fig. 12.2
(a) The use of thermal energy during the dissection of the neurovascular bundles has been proven to result in injury to the nerve fibers and significantly comprise the outcome of the nerve-sparing technique. The image shows the dissection of the neurovascular bundle with the use of ultrasonic scissors during the performance of non nerve-sparing approach. (b) The neurovascular bundle is meticulously dissected with the consecutive use of clips and blunt dissection. No energy instruments are used in the vicinity of the neurovascular bundles
12.4 Oncological Results
The main criterion used to assess the oncological efficacy of radical prostatectomy is the presence or absence of PSMs. Additional factors of interest are the level of post-operative PSA and more specifically, PSA recurrence (described in literature as PSA >0.2 ng/mL and confirmed by a second measurement), the clinical progression and the progression-free survival [4, 50]. Prostate size does not represent a parameter for patient selection to undergo LRP. Nevertheless, prostate sizes smaller than 30 g are related to a higher rate of PSMs [51, 52]. Techniques of nerve reconstruction, such as sural nerve grafting, have been associated with increasing risk of PSMs [53]. Moreover, previous training of the surgeon in open or laparoscopic techniques does not have an impact to the oncological outcome [54].
The learning curve seems to have an impact to the PSM rate according to a recent meta-analysis which showed inferior PSM rates in LRP in comparison to RALP cases performed by surgeons in their learning curve [55]. Other investigators concluded that a surgeon early in the learning curve of LRP probably does not result in increased rate of PSMs [56]. The oncological results of LRP are similar to those of ORP and the PSMs are detected in the same sites in both approaches [4, 56]. Short-term oncological results reported by Salomon et al. showed PSM and 3-year progression free survival rates to be 20.6 and 86.2 % in pT2 cases, respectively. The rates were similar among LRP and ORP [57]. Similar results were also documented by Roumeguere et al. [45]. A comparison of transperitoneal and extraperitoneal approach did not demonstrate any significant difference in PSM rates among the approaches [8, 9].
In a prospective study including 1,000 patients Guilloneau et al. reported progression free survival at 3 years post-operatively. They observed 80 and 94 % progression free survival rates (overall rate 90.5 %) in patients with and without PSMs, respectively. Factors influencing the PSM rates were Gleason Score, clinical stage (TNM), pathological stage and preoperative PSA level [50]. Rozet et al. reported an overall PSM rate of 17.7 % as well as 14.6 and 25.6 % in pT2 and in pT3 cases, respectively [33].
Five-year progression free survival rate of 78.8 % was reported by Goeman et al. in a series of patients who underwent extraperitoneal LRP. PSM rates were 17.9 % for pT2, 44.8 % for pT3 and 71.4 % for pT4a tumors [32]. In a large population of patients Stolzenburg et al. [6] observed overall PSM rate of 16.4 %. The PSM rate for patients in pT2 stage was 8 and 35.6 % in pT3 stage. The long-term results on PSM and biochemical recurrence rates showed that the laparoscopic approach does not compromise the oncological outcome [40, 41, 58].
12.5 Complications
Complication rates for LRP and EERPE range between 2 and 17 % [59, 60]. The Table 12.1 summarizes most frequent complications and management. Vascular complications, including vessel injury, bleeding and the formation of hematomas represent the most common perioperative complications of LRP/EERPE (89.4 % of all complications) and an incidence up to 6 % of all cases has been reported [59–63]. Hemorrhage from the inferior epigastric vessels (during trocar insertion), the Santorini’s plexus, or the external iliac vein are common intra-operative complications [59–63]. Hematomas are also common post-operatively and arise from the NVBs or epigastric vessels. Rectal and intestinal injuries are reported with an incidence of 9 % of the cases and tend to be severe and life-threatening if they are not recognized intraoperatively [59–63].
Complication | Rates (%) | Management | Tips |
|---|---|---|---|
Injury of inferior epigastric vessels | 0–6 | Bipolar coagulation | Careful inspection of all the trocar sites for active bleeding before and after the removal |
Clipping | |||
Suturing of the bleeding vessel on the abdominal wall | |||
External iliac vein injury | Endoscopic repair with 4–0 prolene | Insufflation pressure can tamponade venous bleeding and makes endoscopic repair possible | |
Conversion to open laparotomy | |||
Santorini plexus injury | Increase of gas insufflation to 20 mmHg and bipolar coagulation | Can be avoided by careful ligation of the plexus and careful inspection-coagulation after apical dissection | |
Retraction of the catheter to tamponade bleeding | |||
Bowel injury | 0.47
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





