Chapter 35 Laparoscopic Pelvic and Aortic Lymphadenectomy for Gynecologic Malignancy
Operative indications
Indication for Pelvic Nodal Dissection
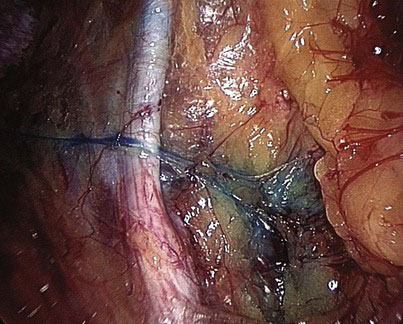
The technique of sentinel node dissection is gaining popularity in gynecologic oncology. Removal of a single targeted node from a node-bearing area can be accomplished with minimally invasive technique. Moreover, the identification of minute lymphatic channels located deep in the pelvis is facilitated with magnification, as provided by the laparoscope (Fig. 35-1). Initial attempts at sentinel node detection involved blue dye injection only, with marginal success; subsequently, combined isotope and blue dye mapping improved the detection rate up to 90%. A sentinel node may be found in an unusual area, such as in the region of the common iliac or aorta. Of note, the sentinel node technique does not apply to obviously diseased nodes in which lymphatic flow is blocked, which would make uptake of markers impossible.
< div class='tao-gold-member'>