Laparoscopic Patch of Perforated Duodenal Ulcer
Sunil Sharma
Bestoun H. Ahmed
The success of medical management of peptic ulcer disease has reduced the overall need for surgical intervention. But, the incidence of perforation, which is a serious and potentially fatal complication, remains the same (5% to 10%). The surgical intervention of simple closure of the perforation with or without omentoplasty is accepted in most of these patients. Modern antiulcer therapy (i.e., H2 receptor antagonists or proton pump inhibitors [PPI] with anti-Helicobacter pylori agents) has decreased the high recurrence rate from 40% to 3–4%.
Laparoscopic patch of perforated duodenal ulcer has become an alternative method to the open procedure since its initial report in 1989 by Mouret. It offers advantages of better visualization of the peritoneal cavity, thorough lavage and lack of upper abdominal incision with its related complications, especially in high-risk patients. The need for definitive surgical procedures is diminishing. However, it depends on the chronicity and intractability of the disease.
Laparoscopic closure is a favorable method in most patients. It is especially indicated in
those with age less than 70 years,
symptoms persisting less than 24 hours,
absence of shock on admission,
American Society of Anesthesiologists grade less than III, and
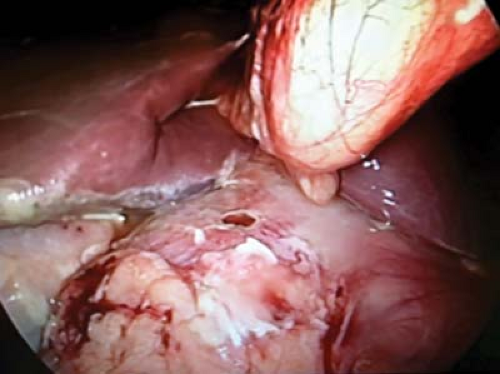
perforation smaller than 10 mm in diameter (Fig. 11.1).
There are no absolute contraindications for the laparoscopic approach. It is preferable to avoid this approach in patients with Boey’s score of 2 or 3. Patients with such a score range are associated with high morbidity and mortality. Boey score (0 to 3) is the count of Boey risk factors: shock on admission, American Society of Anesthesiologists grade III to V, and prolonged perforation. A Boey score of 0 means low surgical risk; otherwise, it is considered a high surgical risk.
Diagnosis is achieved by the history of sudden onset of abdominal pain with abdominal findings indicating peritonitis. Free air under the diaphragm is expected in 85% of patients. Usually, no further diagnostic measures are indicated.
Following diagnosis, the preoperative resuscitation is achieved by intravenous fluids (crystalloids), nasogastric intubation, and urinary catheterization.
Therapeutic intravenous antibiotics should be started preoperatively and continued postoperatively. Once the patient tolerates oral intake, antibiotics will be switched to an oral formula which treats H. pylori organisms.
H2 blockers or PPI should also be started preoperatively and continued throughout the postoperative period.
These patients must be scheduled for urgent laparoscopic exploration.
Diagnostic laparoscopy is indicated in all patients except the minority who present with a high Boey’s score. For this small group of patients, starting with exploratory laparotomy is the safest approach.
Positioning
The patient should be in supine position with sequential compression devices and safety belts on the lower extremities. Both arms should be tucked to allow freedom of movement for the surgeon and assistants.
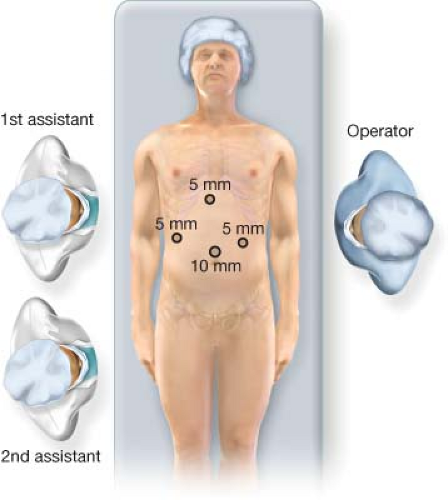
Some surgeons prefer to stand between the patient’s legs while others perform the procedure from the patient’s left side.
Standing on the patient’s right side makes suturing an easier task. But, change of position may be needed to achieve an efficient peritoneal lavage (Fig. 11.2).
Under general anesthesia, the patient is placed in a 15- to 20-degree reverse Trendelenburg position. The operating surgeon stands on the patient’s left. This initial position allows better diagnostic exploration and more efficient peritoneal lavage. An
assistant stands on the right side. Later the surgeon may switch the position to the right side for easier suturing.
All port sites should be infiltrated both subdermally and preperitoneally with 0.5% bupivacaine prior to incision or creation of the trocar path.
Through a 2-mm-long left hypochondrial stab incision just inferior to the costal margin at the midclavicular line, the carbon dioxide pneumoperitoneum (up to 15 mm Hg) is established with a Veress needle.
After establishing the pneumoperitoneum, through a 10-mm-long supraumbilical curvilinear incision a 10-mm trocar is placed and an angled laparoscope with 30° or 45° is introduced and the entire abdominal cavity is thoroughly investigated. If the laparoscopic findings correspond with the preliminary diagnosis of perforated ulcer, additional trocars are placed under laparoscopic view.
A 5-mm port is placed one hand-breadth below the left costal margin at the midclavicular line. This port is used as the right-handed working port and can be used to introduce the ski-needle and suture or could be exchanged for a 12-mm port if a regular curved needle or an Endostitch (Covidien, Norwalk, CT, USA) is used. Another 5-mm port is placed in the right hypochondrium at the midclavicular line one hand-breadth from the liver edge on the abdominal wall below the costal margin. This port is the left-handed working port.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree