Chapter 20 Laparoscopic Management of Pancreatic Pseudocysts
Operative indications
Patient positioning and placement of trocars
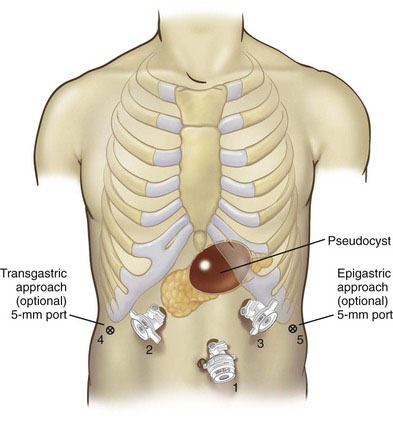
All procedures are performed under general anesthesia, with broad-spectrum antibiotic coverage and prophylaxis against deep venous thrombosis. For laparoscopic pseudocyst-gastrostomy, the patient is placed in the French (lithotomy) position, with the surgeon standing between the legs, the first assistant and scrub nurse to either side, and the monitor over the patient’s head. The surgeon’s position for pseudocyst-jejunostomy may be on either side of the table or between the legs, depending on the PP location. The pneumoperitoneum is set at 12 mm Hg. A 10-mm port for the 30-degree laparoscope is placed one handbreadth away from the target (the PP-gastric or PP-jejunal anastomosis), and two or three 5- or 10-mm ports are placed on either side in order to achieve triangulation (Fig. 20-1). An additional 5-mm port may be placed laterally to retract the liver, spleen, and stomach if these organs impinge on the operative field.
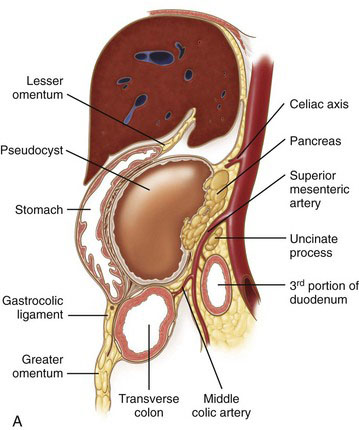
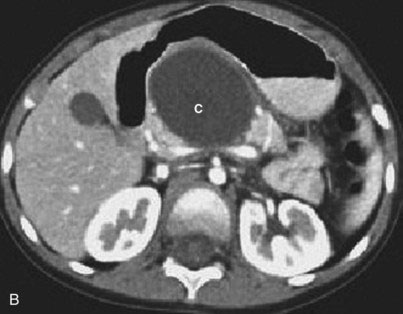
Anatomic classification of pancreatic pseudocysts
The following section describes a surgically oriented approach to the classification of PP disease.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree