Chapter 5 Laparoscopic Esophagomyotomy with Nissen Fundoplication
Achalasia is a rare primary esophageal motility disorder characterized by progressive dysphagia. Although the degree may vary among individuals, dysphagia is present in all patients affected by the disorder. Other symptoms, such as chest pain, epigastric pain, odynophagia, regurgitation, vomiting, heartburn, and weight loss, may also be present. Physiologic features include aperistalsis of the esophageal body, normal to high lower esophageal sphincter (LES) resting pressures, and a lack of LES relaxation on swallowing. Treatments are aimed at relieving dysphagia by disrupting the LES musculature or promoting its relaxation. Short-term relief of dysphagia can be achieved with endoscopic botulinum toxin injections or pneumatic dilations. Endoscopic treatment of achalasia was the preferred method in the 1970s and 1980s despite many reports showing the superiority of an esophagomyotomy over dilation. Esophagomyotomy was first described by Heller in 1913 and later modified to a single anterior myotomy. Although the thoracic approach has been widely used to perform the myotomy, the abdominal approach has emerged as the preferred approach by the surgical community. In cases of reoperative myotomy due to incomplete proximal myotomy or a hostile upper abdomen from previous surgeries, the thoracic approach may be useful. Laparoscopic esophagomyotomy was popularized in the 1990s and has become the treatment of choice for patients with achalasia. Long-term relief of dysphagia in the 90% range, minimal postoperative pain, short hospitalization, and overall patient satisfaction contribute to its wide acceptance. Symptoms of postoperative reflux, which can be as high as 60%, can be reduced with the addition of a fundoplication. A balance must be maintained between controlling reflux and avoiding a significant increase in resistance caused by the fundoplication to an aperistaltic esophageal body. The superiority of the complete (Nissen) wrap over partial (Dor, Toupet) wrap in controlling reflux symptoms has been well demonstrated in the treatment of gastroesophageal reflux disease (GERD). The decision to perform a partial versus a complete fundoplication remains controversial, although most fundoplications performed after a myotomy are partial. Several reports show an increased incidence of dysphagia with a complete fundoplication compared with a partial fundoplication. We believe the difference in dysphagia rates represents technical error of the fundoplication rather than a significant difference in the resistance of the complete wrap. We routinely perform a short floppy Nissen fundoplication after an esophagomyotomy with a low incidence of postoperative dysphagia. On the accompanying DVD (as well as on Expert Consult), we have included a video of a laparoscopic esophagomyotomy with Nissen fundoplication as an update and contrast to the procedure described in Chapter 2 of the Atlas of Minimally Invasive Surgery, 2009 (see Suggested Readings at the end of this chapter). The fine dissection and tips described here are the result of years of experience of the senior author (CTF), and we hope the viewer will gain the valuable insight necessary to perform the operation successfully.
Positioning and placement of trocars
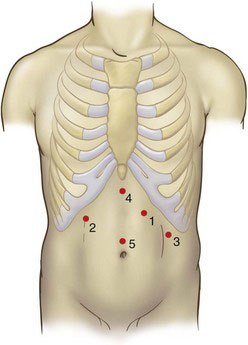
The patient is placed in modified “French” lithotomy position as shown in Figure 5-1 with 30-degree reverse Trendelenburg. The surgeon stands between the patient’s legs, the camera operator stands to the patient’s right, and the first assistant stands to the patient’s left. Five trocars are placed as shown in Figure 5-2. The initial port (number 1) is placed using the optical trocar in the left midclavicular line subcostally and serves as the surgeon’s operating right hand. Subsequent trocars are placed in the order numbered two through five. The basic principles of trocar position and use should be followed: the camera port (number 5) should be in the midline superior to the umbilicus. The surgeon’s left-hand working port (number 2) is placed in the right subcostal region in the midclavicular line. The retraction and assistant port (number 3) should be placed in the left midaxillary line caudad to port number 1. Trocar number 4 is used to retract the left lateral lobe of the liver and is placed in the subxiphoid region.
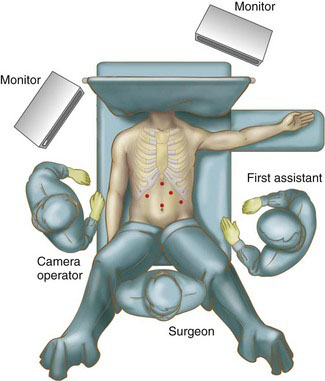
FIGURE 5-1 Patient positioning and operating room layout for the performance of laparoscopic esophagomyotomy.
Operative technique
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree