Chapter 25 Laparoscopic Colectomy for Diverticulitis
Operative indications
In this chapter, the technique for laparoscopic sigmoid colectomy with primary anastomosis in a complex case of diverticulitis is described. On the accompanying DVD (as well as on Expert Consult), we have included a video demonstrating the case of a patient with a history of multiple previous episodes of diverticulitis. The patient presented with a more severe recurrent attack, failed conservative treatment with percutaneous drainage of an abscess and intravenous antibiotics, and developed a colovesical fistula. The incidence of fistulas in patients with diverticular disease, the most common cause of colovesical fistula, is accepted to be 2%, although some centers have reported higher percentages. Colovesical fistulas are more common in males. Women who present with colovesical fistulas are commonly older or have a history of hysterectomy. The diagnosis is made clinically and confirmed with cystoscopy. This acute case can be compared with the case described in Chapter 15 of the Atlas of Minimally Invasive Surgery, 2009 (see Suggested Readings at the end of this chapter), in which the patient was successfully treated with antibiotics and the inflammation subsided before resection.
Patient positioning and port placement
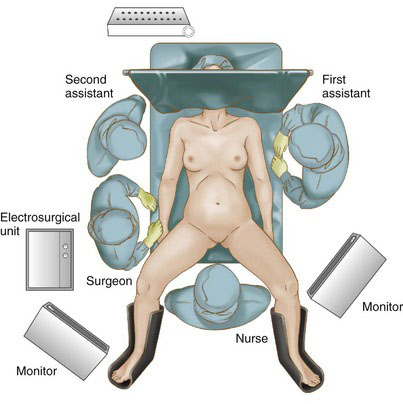
For a laparoscopic sigmoidectomy, the patient is placed in the low lithotomy position with stirrups (Fig. 25-1). This positioning allows the end-to-end anastomotic (EEA) stapler to be used per the rectum. The left hip is elevated off the operating table by using a beanbag, viscoelastic cushion, or similar device. Placement of bilateral ureteral stents by a urologist, in particular infrared-illuminated stents (InfraVision, Stryker, San Jose, Calif.), is helpful in identifying the ureters when dealing with the phlegmon and inflammation of diverticulitis.
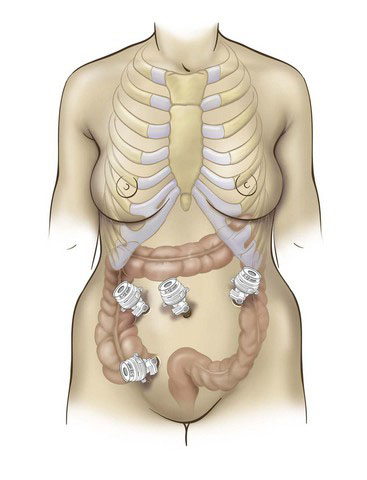
The surgeon stands on the patient’s right, facing a monitor. The authors prefer to access the abdomen using the open Hasson technique inferior to the umbilicus. This incision can then be extended to remove the specimen. If the patient has had previous surgeries, it may be prudent to insert a bladeless optical trocar at a different site to access the abdomen. After the pneumoperitoneum is established, two additional 12-mm trocars are placed in the right abdomen, just inferior and superior to the level of the umbilicus (Fig. 25-2). The use of 12-mm trocars at all port positions allows for maximal instrument flexibility. The placement of additional trocars may be necessary depending on the extent of the operation and the complexity of dissection. There are no set rules for the perfect port positioning. The surgeon must carefully consider each trocar placement in relation to the dissection and also to the other trocars. The main reason for conversion to open is the malpositioning of the trocar sites.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree